strategic skill builders:
A FREE CONTINUING EDUCATION SERIES
New Empirical Suggestions
for Prescribing Soft Toric Contact Lenses
How to get the right
fit the first time.
BY LORETTA B. SZCZOTKA, O.D., M.S., F.A.A.O.
Empirical fitting is the best way for many O.D.s to decrease chair time and avoid trial lens sterilization and the need to stock multiple trial lens sets. Fitting from an available trial lens set is considered an "empirical fit" if, by following empirical fitting guidelines, you can achieve first-time success without having to try multiple lenses. I'll explain what to do.
SELECT THE RIGHT PATIENTS
The first step in successful empirical lens fitting is to select the correct patients. Very simply, a soft toric lens candidate is any patient who has a regular refractive sphero-cylindrical spectacle prescription.
General guidelines. Traditionally, astigmatic patients who were fit with toric lenses had a refractive cylinder between 1.00D and 2.50D. However, now patients with both low cylinder (0.75D) and higher cylinder (up to 9.75 D) can benefit from disposable or planned replacement options.
Despite the fact that at least seven manufacturers make 2-, 4- or 12-week disposable lens options for them, many patients with 0.75D are still fit with spherical hydrogel lenses. If these patients -- especially early presbyopes -- have symptoms of blur, fatigue, asthenopia, accommodative spasms or accommodative insufficiency with spherical lenses, they're excellent candidates for soft toric lens vision correction.
Lenticular astigmatism patients. These are excellent candidates for soft toric lenses because a rigid gas permeable (RGP) lens will do little to correct the residual astigmatism with a tear lens.
A quick glance at a patient chart can easily help you make your recommendation. Patients who have refractive astigmatism and spherical keratometry readings or topography maps have internal astigmatism and won't visually benefit from a spherical rigid lens. Internal astigmatism is usually lenticular and often against-the-rule (ATR); these patients require cylindrical lens correction such as a soft toric lens.
Unilateral, occasional contact lens wearers or previous dropouts. The occasional or unilateral contact lens patient will stop wearing lenses altogether if each lens insertion requires re-adaptation or excessive cleaning regimens.
Modern soft toric programmed replacement and disposable lenses are thinner, resistant to deposit formation, easier to care for and more comfortable compared with older torics. New "low-torque" designs decrease the lens rotation that used to cause fluctuating vision, and if a lens is rotated, new stabilization techniques will return it to its baseline position in a matter of blinks rather than minutes.
Try approaching unilateral or social contact lens wearers again. Improved comfort and minimized lens awareness will lessen or eliminate the discouraging lens adaptation they used to have to endure.
Critical visual acuity needs. Probably the most important subgroup of patients to consider for soft toric lens correction is those who have critical visual acuity needs. In addition to spherical soft lens patients who have symptomatic residual astigmatism, patients who have critical acuity needs include those who routinely:
- perform detailed reading and near work
- use a computer
- drive at night
- require monovision.
Monovision. Since monovision decreases stereopsis and diminishes binocular overlap, these patients require optimal monocular visual acuity. Fitting them with spherical soft lenses and ignoring even 0.75D of cylinder may be acceptable for those who have balanced binocular function. However, when the additive effect of the other eye isn't available, I only recommend lenses that help my patients achieve their best potential monocular acuity.
Most monovision patients complain of diminished distance vision with monovision lens use from the visual overlap of the near image. Interestingly, their near visual acuity is usually acceptable and they welcome the change away from reading glasses.
Additionally, un-corrected cylinder is less symptomatic in the near eye and even provides some additional near lens power if in minus cylinder form. Hence, allowing uncorrected cylinder in the near eye in a soft lens astigmatic monovision fitting may be acceptable, but you should fully correct the fellow eye so that the patient has the proper distance function.
The distance eye (usually the dominant eye) is best served with a soft toric lens (if residual astigmatism is present over a spherical soft lens) to allow the patient to perform the critical distance tasks that are required in driving and in sports with the least amount of visual compromise.
Dry eye patients. Patients who have physiological dry eye usually succeed in a prism ballast design, presumably because of an increased center thickness and base, which may help retain water and limit dehydration.
Also, some experts claim that prism ballast soft lenses help with tear retention on the eye by increasing the inferior tear meniscus and promoting better tear pooling.
BEGINNING THE EMPIRICAL FIT
Once you've chosen the correct candidate, the focus changes to selecting the best contact lens design. Traditional thinking was to prescribe a back surface toric lens for true corneal astigmatism patients because, theoretically, this design should align along the major meridians of the cornea for a "hand-to-glove" fitting relationship. However, this method of lens selection isn't widely practiced.
Often front surface toric lenses work well on toric corneas, and back surface toric lenses work well on spherical corneas.
Manufacturers all have suggested using nomograms when ordering lenses empirically or when selecting the first trial lens based on manifest refraction and keratometry. Howev-er, our estimate of empirical ordering (first lens) success rates is approximately 62%. Success rates can run as high as 91% when you reorder the first contact lens based on clinical evaluations and corrections of unexpected physical fitting relationships and unanticipated power errors.
We believe that these residual fitting difficulties exist because soft toric lens fitting recommendations use only keratometric data to estimate curvature selection and to predict on-eye lens performance. We think that corneal topography, a state-of-the-art method for measuring corneal curvature, can determine the optimal empirical fitting and therefore the initial success rates of soft toric contact lenses.
CORNEAL TOPOGRAPHY MAPS
Typically, clinical practice uses placido-based topography systems, which employ a series of illuminated annular rings projected onto the cornea. Using the corneal tear film as a mirror, a digital video camera captures the reflected image of the rings. The image is then subjected to an algorithm to detect and identify the position of the rings relative to the videokeratographic axis.
Some thin ring projection systems such as the TMS-2 (Tomey Technology), Humphrey Atlas (Zeiss Humphrey Systems) and Keratron (Optikon 2000) use a peak luminace algorithm where the brightest portion (the center of the ring) is identified as the border.
Wide-ring projection systems such as the EyeSys 2000 (EyeSys/ Premier) and CT 200 (Paradigm Medical Industries) use a border detection algorithm to detect both edges of each illuminated ring. Once the borders are detected, a proprietary algorithm is applied to the digital image, which "reconstructs" the corneal curvature.
Corneal topography has already successfully incorporated RGP fitting nomograms into the software packages for quantitative contact lens parameter selection. Someday, we'll also have sophisticated software packages that will troubleshoot soft toric lens fitting. For now, you can retrieve some of the most important fitting information for soft toric lenses by viewing the standard map displays.
However, you need to have a good understanding of corneal topography maps because the many variations of curvature maps can confuse or overwhelm those who are trying to incorporate this into everyday practice.
CURVATURE MAP OPTIONS
Curvature map options vary in how they apply a mathematical function to the raw data. The most common maps used for contact lens practice are:
- the tangential radius of curvature representation (also referred to as instantaneous, local or true map)
- the axial representation (also referred to as sagittal, color or default map).
Differences between the two representations become greater for corneal points in the mid-to-far corneal periphery. This results in many clinically significant differences relevant to contact lens fitting, especially when you're looking for specific patterns and corneal shapes for describing the different forms of corneal toricity.
|
|
|
|
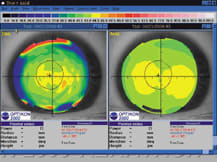
Figure 1. Curvature map differences for a keratoconus eye.
The figure on the left is a tangential mechanism. |
|
Figure 1 shows curvature map differences between axial and tangential displays for a keratoconus patient, highlighting greater differences in the corneal periphery.
The axial map is based on a spherically biased algorithm that closely mimics keratometry measurements. It was intended to simulate refractive power in the corneal "cap," the supposedly spherical portion of the cornea.
The tangential representation produces "true" curvatures based on a standard definition of the local curvature at a given point along a curve. Therefore, tangential maps provide a more accurate description of corneal shape.
Tangential maps also include extreme curvature values, offering a more detailed view of localized corneal curvature. Therefore, tangential curvatures of a relatively flat area of a cornea will appear flatter than the respective axial value, and relatively steep areas will be imaged as steeper on tangential maps compared to their axial counterparts.
Finally, tangential maps will provide the same relative shape patterns as the axial counterpart, but the patterns will be smaller and confined more to the central area of the map. This quality creates a critical difference when you're classifying the astigmatic corneal shapes relevant to soft toric lens fitting.
|
|
|
|
Figure 2. Curvature map differences for an astigmatic eye. The map on the left figure is the tangential; right is the axial display. |
See Figure 2 for an example of the different patterns you may find when looking at a corneal with-the-rule astigmat on axial and tangential maps.
USING CORNEAL TOPOGRAPHY TO FIT SOFT TORIC LENSES
Recently we investigated topography for possible influences on the fitting of soft toric contact lenses. We wanted to determine whether corneal topography could provide indices to predict which eyes would succeed with empirical fitting utilizing the current fitting guidelines, and which may require using new nomograms.
We're a long way from beginning to recommend new parameters for every soft toric lens based on the patient's topography. However, we've made some advances that we can translated into clinical applications. The results of our analyses will eventually be used to suggest updated nomograms for soft toric empirical fitting based on a patient's baseline corneal topography.
THE HYPOTHESIS
Our working hypothesis contends that lens flexure alters the lens back vertex power (BVP) in situ, which is currently unpredictable by most standard mechanisms of ocular assessment.
For appropriate vision correction with a toric soft contact lens, the BVP in situ of the contact lens on the eye should be equal to the patient's refraction at the ocular plane.
If a toric soft lens doesn't rotate when placed on the eye, then the specified BVP will be the same as the BVP in situ, provided that no significant tear lens forms under the soft contact lens and that the degree of lens flexure is negligible.
However, previous studies have demonstrated that lens flexure does occur in soft toric lenses, and this will alter the lens's on-eye fitting and power characteristics.
We hypothesized that soft toric contact lens performance -- presumably because of flexure -- varies, depending on the corneal topography of patients who have differing amounts and forms of corneal astigmatism. But what are these different forms of corneal astigmatism? I will discuss that next.
TYPES OF CORNEAL ASTIGMATISM
After examining hundreds of eyes with refractive astigmatism, we recognized 5 classic types:
- Type I (spherical cornea): <0.75 D central and peripheral astigmatism; refractive astigmatism is therefore lenticular.
- Type II (central astigmatism): >0.75D central astigmatism: at least 0.75D more corneal toricity centrally than peripheral toricity.
- Type III (limbus-limbus equal astigmatism): central astigmatism within 0.75D of peripheral astigmatism.
- Type IV (limbus-limbus greater peripheral astigmatism): peripheral astigmatism is greater than central astigmatism; difference >1.00D.
- Type V (limbus-limbus irregular peripheral astigmatism): peripheral astigmatism irregular; opposing hemi-meridians vary by >3D.
To classify the forms of corneal topography yourself, you'll need to record certain data points obtainable from your corneal topography instrument's tangential maps.
You need the tangential maps because they more accurately depict the corneal shape.
Begin by obtaining measurements at a 3.5 mm radius from the center of the map along the flat and steep corneal meridians as defined by the Sim K data, and compare this to the Sim K suggested astigmatism to obtain the classification.
The individual steps are as follows:
1) Record two points 3.5 mm away from the center of the map, 180 degrees apart, on the flat meridian and average them.
2) Subtract this value from the average of the peripheral points at a 3.5 mm radius along the steep meridian to give a measure of peripheral corneal astigmatism.
3) Obtain central astigmatism from the Sim K data reported by the instrument.
4) Classify the astigmatism into one of the 5 types above based upon differences in central and peripheral corneal toricity.
WHAT TO EXPECT WITH DIFFERING FORMS OF CORNEAL TORICITY
To our knowledge, we're the first to use some measurement of peripheral corneal toricity as an indicator of soft lens performance. In our study, we fit 149 patients empirically with prism ballasted back surface toric soft lenses per the manufacturer's fitting guides.
We then performed statistical analysis to assess associations between empirical fitting success and the form of corneal astigmatism, and to assess the differences between success and failure groups in numeric topographic variables.
Our results revealed that you can anticipate soft toric fitting success with certain forms of astigmatism, specifically in eyes that have spherical corneas (remember, soft toric lenses on spherical corneas correct lenticular astigmatism), central astigmatism or corneas that have peripheral toricity that matches the central toricity (Types I, II, and III).
Other eyes had higher or irregular peripheral corneal astigmatism and much lower empirical fitting success rates.
|
|
|
|
Figure 3. Here's an example of central astigmatism on tangential and axial displays. |
|
Our data also revealed that peripheral corneal toricity occurs in most astigmatic patients. Specific-ally, 66% had high or irregular peripheral corneal toricity. These eyes are at risk for lens flexure, which can result in unanticipated fitting and power errors.
If you detect toricity proactively with topography, your approach to patient management could change.
For example, if you anticipate an empirical fitting failure based on current manufacturer nomograms, you could initiate a diagnostic fitting rather than rely on an empirical order.
The surprising finding was that peripheral toricity occurs in most patients; therefore this detection mechanism of eyes predicted to "fail" empirically with the first lens is significant.
|
|
|
|
Figure 4. Example of limbus-to-limbus full corneal astigmatism on tangential and axial displays. |
Clinically, the best way to quickly recognize which eyes will succeed or fail is to mentally refer to an eye as having central or total corneal/ peripheral astigmatism (see Figures 3 and 4).
The image in Figure 3 shows an eye that has oblique central astigmatism. The image in Figure 4 shows a cornea with total limbus-to-limbus astigmatism.
The eye in Figure 4 (see below) has a greater chance of failing with the first empirically ordered contact lens, presumably because of lens flexure with unanticipated power errors. Therefore, I'd either initiate a diagnostic fitting in the second patient or recommend using an RGP contact lens.
LOOKING AHEAD
Studies are already underway into using topography data to im-prove empirical success rates in first-time fitting so they're comparable to those achieved in second and third time re-orders.
These studies also seek to quantitate the topography data with new indices to predict success and failure utilizing currently available nomograms. This information will help decrease valuable chair time in eyecare practices and also decrease lens usage, thereby increasing the efficiency and efficacy of soft toric lens fitting.
Dr. Szczotka is an associate professor at Case Western Reserve University Department of Ophthalmology and is director of the Contact Lens Service at University Hospitals of Cleveland in Cleveland. She's a Diplomate in the Cornea and Contact Lens Section of the American Academy of Optometry and lectures and publishes nationally and internationally.
References can be made available upon request