|
|
|
Coordinated by Bobby Christensen, O.D., F.A.A.O. |
therapeutic insights
Coping with Complications
Part two of a two-part series on
treating laser vision corrections.
By Jason Ellen, O.D., Tulsa, Okla.
Last month, I explored two complications that are common following laser-assisted in situ keratomileusis (LASIK). This month, I'll finish the discussion by reviewing two more complications (dry eye and striae) that you may encounter.
Dealing with dry eye
One of the most common complaints after LASIK is that of dry eye syndrome (DES). In many of these cases the symptoms were not present before surgery. The first step in treating post-op DES is to diagnose and treat any pre-op signs and/or symptoms.
Because LASIK can exacerbate minor dye eye conditions by reducing the blink reflex, decreasing corneal sensitivity and increasing inflammatory mediators within the cornea, it's important to ascertain the patient's baseline tear production and corneal health before surgery. Make sure to educate patients who are taking antihistamines, hormone therapy or anticholinergics about the need for temporarily discontinuing the medications or frequent lubrication after LASIK. Also address any signs of meibomian gland dysfunction.
|
PEARLS FOR DRY EYE COMPLICATIONS |
|
|
|
Caring for lens wearers
Be cautious of patients who are considering LASIK because of the dryness they experience from wearing contact lenses. Make sure the symptoms subside after cessation of contact lens wear. Patients who have high prescriptions, low Dk lenses or who are in extended wear lenses are more likely to have corneal hypoxia. These patients should have a longer deadaptation period to allow the corneal sensation to return to baseline. Unfortunately, pre-existing DES conditions may go undetected before surgery and therefore become even more problematic after surgery.
Patients who undergo LASIK and show signs of DES most often respond to aggressive use of preservative-free artificial tears. Some studies have shown that tear supplements that contain carboxymethylcellulose (Celluvisc and TheraTears) provided better relief and increased compliance for post-op patients. Another study found that Thera Tears increased goblet cell density in dry eye patients. For those who need more than artificial tears, consider punctal plugs.
Managing severe cases
A mild steroid (Flarex, FML) used t.i.d. or a high-Dk bandage contact lens can help "turn" a fairly severe dry eye. For severe cases, always rule out systemic, drug and adnexal causes.
In some cases it may be necessary to treat patients with Human Albumin extract. This is a fairly expensive alternative that you usually have to have a hospital pharmacy compound, but it can be an excellent "last chance" alternative for these patients.
Recent studies suggest that damage to the corneal epithel-ium and/or the dissection of the corneal nerves lead to LASIK-induced neurotrophic epitheli-alopathy (LNE). This may help explain the patient who reports moderate dry eye symptoms but has no objective signs of epithelial damage.
In many of these cases, artificial tears temporarily relieve the symptoms until the corneal nerves re-innervate the lamellar flap, which usually takes 3 to 6 weeks. For the small group of patients who have persistent DES, I've found that cyclospor-ine A 0.1%, formulated in TheraTears, provides relief in roughly 75% of these patients. This is dosed t.i.d. for 2 to 3 weeks and then tapered over 1 month.
Struggling with striae
Striae, which are characterized by large wrinkles or actual folds within the corneal flap, are detectable with direct illumination. Striae within the LASIK flap can be as benign as a faint peripheral microstria that has no impact on visual acuity, or severe as an accordion-shaped fan of striae encompassing the entire flap resulting from flap dislocation.
When a patient presents with a flap dislocation caused by trauma (or, more likely, rubbing his eye soon after surgery or during the night), the diagnosis and decision to refer for surgical treatment is easy. It's when the flap (on first inspection) appears clear and the patient complains of mild blur or ghosting that diagnosis and the decision for treatment becomes more difficult.
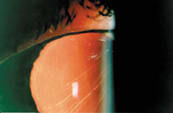
Using retro-illumination through a dilated pupil can enhance the detection of minor striae (small wrinkles in the corneal flap) significantly. Fluorescein stain helps enhance areas of microstriae by pooling within the small indentations. This pooling is usually more apparent 30 to 45 seconds after instillation when most of the stain has drained from the eye.
When trying to determine if barely visible striae are visually significant, watch for induced hyperopic astigmatism in which the axis is oriented 90š from the line of the striae. Also look for topographical changes such as irregular astigmatism or areas of elevation within or near the pupil.
|
|
|
| Direct and indirect illumination of multiple central and inferior striae. | Retroillumination of striae because of flap rotation. |
Managing severe cases
When patients do present with visually significant microstriae, early treatment is essential. The longer a stria is present within the collagen, the harder it is to remove by stretching the flap. Surgical treatment of striae may be as non-invasive as to "squeegee" it from the center of the flap to the periphery.
This procedure can be performed at the slit lamp using forceps or a specialized instrument called a Kornmell press, which is specifically designed to press and roll the striae to the outer edge of the flap.
|
|
|
|
Direct illumination of multiple central and peripheral striae caused by movement of the flap. |
|
For significant striae, most surgeons prefer to lift and stretch the flap. The surgeon lifts the flap past the point of the striae and replaces it. He then begins to stretch the flap by pressing from the center to the outer edge, continuing until the epithelium is dry enough to attain significant traction.
In some cases, the surgeon will completely remove the epithelium to gain enough traction to effectively stretch the flap.
In extremely severe cases, or cases where an initial lift and stretch didn't attain the desired effect, suturing the flap with 10-0 sutures may be required to maintain enough "pull" on the flap to remove the striae.
Identifying striae risk
It's important to identify scenarios in which a patient is at increased risk for developing striae or microstriae. To help you in the future, watch for the following specifics:
- patients who have high refractive corrections (hy peropic or myopic)
- poor compliance (rubbing, not wearing shields and "winking" to check visual acuity unilaterally)
- patients who have thin flaps (130µm to 160 µm)
- corneal/flap swelling (Sands)
- early endothelial changes or Fuch's dystrophy
- pre-existing dry eye
- poor initial placement of the flap.

Wishing future success
Hopefully now you're more confident about comanaging LASIK patients. If you encounter a complication, you'll know it's most likely one of the four I discussed in this column and you'll be better armed to treat it.