strategic skill builders
A Free Continuing Education Series
|

|
|
|

|

|
|

Stanley J. Yamane O.D., F.A.A.O. Vice President, Professional Affairs
|

Howard B. Purcell O.D., F.A.A.O. Director, Professional Affairs
|
Dear Colleague,
Vistakon, Johnson & Johnson Vision Care, Inc., the world's largest manufacturer of contact lenses, is proud to sponsor the 2004 Strategic Skill Builders Continuing Education (CE) Series. Support of eye care education is a high priority at Vistakon. We sincerely hope you find these CE modules to be useful educational tools in your optometric practice.
Optometric CE certification is provided by the Irving Bennett Business and Practice Management Center at the Pennsylvania College of Optometry. Because CE requirements and correspondence credit rules vary from state to state, we advise you to check with your state board to determine if these modules have been approved.
Today's healthcare environment is exciting and dynamic. New developments are occurring almost every day, challenging us to stay abreast of new clinical and practice management information. To meet the challenge, we must continue the learning process throughout our lives because doing so keeps us on the cutting edge, paying big dividends in terms of benefits to our patients and practices.
We want to acknowledge the hard work and dedication invested in this project by the authors of these modules and the outstanding Optometric Management staff.
We hope you take advantage of this educational opportunity. It's just one of the ways Vistakon wants to help you provide the best possible care to your patients. Certainly, that's a goal we can all share.
With warmest regards,
Stanley J. Yamane and Howard B. Purcell
This Strategic Skill Builders Continuing Education article is made possible by a grant from Vistakon. The content is independently produced by Optometric Management.
Fitting Lenses Post-Op
This primer will walk you through the basics of fitting contact lenses after corneal and refractive surgery.
BY COLLEEN RILEY, O.D., M.S., AND JOEL A. SILBERT, O.D., F.A.A.O.
Surgical complications after refractive surgery can and do occur, and patients may require contact lenses to restore their acuity or to reduce distortion. This article will review the many post-surgical applications of contact lenses as well as the complications you can anticipate and address with contact lenses.
ALLOW TIME BEFORE FITTING
Before you fit a post-surgical patient with contact lenses, make sure he demonstrates refractive and corneal physiological stability (although this may not be possible for some). For incisional surgery such as radial keratotomy (RK) or astigmatic keratotomy (AK), you should leave a three- to four-month interval before fitting contact lenses. With LASIK, the interval is at least six months and for PRK it's eight to 12 months. It's necessary to adhere to these intervals to allow for full corneal healing, to prevent the contact lens itself from triggering corneal haze formation and refractive regression (with PRK), and with LASIK to allow adequate time for adherence of the flap to the underlying stroma. Waiting the appropriate time also lets you establish a refractive baseline.
Although patients who require contact lens treatment after refractive surgery are anxious to have visual acuity restored, many have had multiple procedures and as such have corneas that need even more time to stabilize. These patients also appreciate contact lens fitting more after such intervals, and they often note dramatic improvement in their visual performance.
First we'll take a look at some of the post-excimer laser applications of contact lenses.
USING LENSES POST-EXCIMER
Post-surgical complications that benefit from contact lenses include:
Corneal haze or scarring. Most likely a PRK complication, where the corneal irregularity it causes can benefit from a GP lens.
Large astigmatic errors. Depending on the amount and location of irregularity, a large standard tricurve, aspheric or keratoconic design may be appropriate.
Undercorrection and overcorrection. Sometimes it's best to deal with undercorrections or overcorrections surgically, but occasionally we'll encounter circumstances in which the patient declines further treatments or the surgeon doesn't recommend further surgery. In such cases, you may find fitting soft or GP lenses relatively uncomplicated.
While GP lenses present challenges because of the cornea's unusual post-surgical oblate shape, soft lens fitting is relatively straightforward. In cases where the patient can achieve good spectacle acuity, you can fit soft lens spheres or torics successfully. Generally, thinner lenses may drape better over the altered corneal surface, but you can find success with many fitting options.
Irregular astigmatism/irregular surface. Subjective complaints of ghost images or diplopia and poor corrected acuities with spectacles may all result from an irregular corneal surface. Cases of significant irregular astigmatism will require a rigid lens to achieve best vision, with the lens supplying a uniform front surface and the tear lens masking the corneal irregularities.
Refractive surgery highly alters corneal topography. Because the typically prolate corneal shape (positive e-value with the cornea steeper centrally, flattening peripherally) becomes oblate (flatter centrally, steeper peripherally), after these procedures, centration almost always requires the use of large diameter lenses, typically in the 9.6 mm to 11.0 mm range. It's nearly impossible for a spherical base curve lens to both align with the post-surgical central cornea and to provide any semblance of centration, as the lens would fit too flat and loose. Thus, experts recommend fitting the mid-peripheral cornea using either pre-surgical K readings or taking post-surgical mid-peripheral K readings (using fixation dots placed on the keratometer or corneal topography).
The goal is to produce a reasonably well-centered lens that demonstrates an alignment fluorescein pattern throughout the midperiphery with central apical pooling (reflecting the flattened central corneal curvature) and adequate edge clearance. To provide good centration, we generally need large diameter lenses or lenses that have large diameters with reverse geometry designs, which is discussed below.
In a study of 10 patients who were fit with GP lenses after PRK, Astin, et al., found optimal results for most patients who had base curves 0.1 mm steeper than the mean K reading, especially when they used diameters of 9.2 mm to 10.0 mm. Interestingly, the researchers refit nearly 50% of these patients from regular GP lenses into soft lenses, despite the fact that the GP lenses provided better visual acuity. Apparently comfort is a primary consideration in the long-term management of these patients. As such, reverse geometry designs have been crucial in making GP lenses the modality of choice for refractive surgery patients, as they can provide much improved comfort and acuity enhancements over regular GPs.
Managing corneal ectasia. Corneal ectasia is a relatively rare post-surgical complication seen with LASIK. It occurs when the stromal bed under the flap is too thin, generally as a result of overly aggressive LASIK treatments. The weakened cornea progressively thins, with the irregularity greatest on the posterior surface. This post-surgical form of "posterior keratoconus" distorts the anterior surface as well, often resulting in greatly reduced best corrected spectacle acuity.
In this situation, a rigid lens will provide the best vision. As this resembles keratoconus, lenses fit in any of the various keratoconic designs perform best. The final acuity, while much better than that attained with spectacles, may not be as good as that generally attained for standard keratoconic fits. This is presumably because of the irregularity being greater on the posterior surface so that the contact lens and the tear lens aren't eliminating the distortion as effectively as in normal keratoconus.
Dealing with decentration. Decentration of the ablation of 1.0 mm or more can produce clinically significant symptoms including glare, halos and/or starburst effects. Although some may attempt to retreat for decentration complications, either by ablating adjacent tissue or by increasing the treatment zone, additional surgery may compound and worsen the condition.
Contact lens treatment may be the patient's best option to enhance his visual acuity and to reduce or eliminate ghosting and irregular images. Generally you'll best achieve this by fitting GP lenses with large diameters and large optic zones.
FITTING THE OBLATE CORNEA
Because myopic refractive surgical procedures create an oblate cornea, these eyes do much better with lens designs that better approximate this new corneal shape. Reverse geometry or "plateau" lens designs have secondary and midperipheral curves that are steeper than the base curve. These lenses usually have large diameters and small optic zones (typically in the 6.0 mm to 6.5 mm range). Secondary curves may be 2.00D to 4.00D steeper than the lens base curve radius.
Reverse geometry lenses are ideal for patients who have undergone myopic refractive surgery and require post-surgical contact lenses. If you don't have access to a large array of diagnostic lenses, then using corneal topography and contact lens design software, you can have your labs design an initial diagnostic lens. In other cases, GP finishing labs may send diagnostic lenses based on keratometric and refractive data that you supply.
USING ALTERNATIVE DESIGNS
You may find a special lens design helpful in treating patients who have irregular astigmatism or decentered optic zones. For example, the stable optics of certain GP materials essentially eliminates irregular astigmatism.
To prevent lens binding and to promote tear exchange, the lens is fenestrated near the limbal region. You can order the lens in a variety of peripheral curvatures, e-values and widths, but experts recommend a starting e-value of 0.8. A tighter peripheral fit with a 0.6 e-value or a looser fit with a 1.0 e-value are available. This design is also useful for a wide variety of conditions where conventional GP lenses fail (e.g., keratoconus, pellucid marginal degeneration, post-PK, etc.).
LASIK patients who need treatment for correction of hyperopia and who demonstrate post-surgical irregular astigmatism still have a prolate shape to their corneas. They may have steeper-than-normal central curvatures, which you can usually treat successfully with GP lenses using steeper spherical base curve values. You can even employ smaller lenses for these patients, and sometimes steeper-fitting keratoconic lens designs may prove helpful.
|

|
|
|
A GP lens fit on a post-RK eye. |
|
FITTING LENSES AFTER RK
After RK or other incisional procedures, you may want to fit the patient with soft lenses or GP lenses. The next sections detail each option.
K Soft contact lenses. Most practitioners prefer GP lenses for post-RK patients, but with careful assessment and the judicious use of materials and lens designs, soft lenses can prove successful in a number of cases. Thin, disposable lenses often produce a better visual result because they drape more easily over the new flattened corneal contour.
Extended wear is contraindicated, as even minimal hypoxia may trigger neovascularization along the incision lines. Later RK techniques in which incisions avoid the limbal plexus have greatly reduced the risk of vascularization with daily wear soft lenses, as does the use of high-Dk silicone-hydrogel materials.
You must also closely monitor these patients when they're wearing soft lenses because of the significant risk for vessel encroachment. Caution these patients to follow wearing time guidelines and to avoid overnight wear.
Gas permeable lenses. For RK patients who require post-surgical lenses, GPs remain the modality of choice. As many of these patients suffer from irregular astigmatism, the benefits of GP lenses in restoring near normal levels of presurgical visual acuity are paramount.
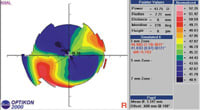
Corneal topography is extremely helpful in evaluating the peripheral corneal contour, which is steeper than the central cornea, when selecting the initial base curve for diagnostic evaluation. Keratometry readings, in contrast, are of little value for this purpose.
You may sometimes want to use conventional GP spherical and aspheric designs, but centration difficulties usually require large diameter lenses (9.4 mm to 10.0 mm). As with post-LASIK GP fitting, reverse curve geometry lenses offer the best chance of centered, stable lenses. A good lens fit will demonstrate central pooling, midperipheral bearing and peripheral edge clearance when you assess it with sodium fluorescein.
|
|
|
|
|
A post PK patient who has high corneal toricity. |
EMPLOYING LENSES POST-PK
In penetrating keratoplasty (PK), the surgeon replaces the majority of the host cornea with a donor cornea, typically using graft sizes between 7.5 mm and 8.5 mm. Experts estimate that up to 50% of patients who undergo PK will require postoperative contact lens care for conditions of high corneal astigmatism (regular or irregular), graft tilt and anisometropia.
The epithelium becomes intact within a few days post-op, but the cornea as a whole may take 18 to 24 months to heal completely. In most cases, it's best to wait at least six to nine months before initiating contact lens treatment. GP lenses offer excellent oxygen transmission and can correct astigmatism and smooth out irregular corneal surfaces. You may also employ spherical or toric hydrogel lenses when fitting the post-PK eye, but you must observe the patient closely to ensure good lens movement and to evaluate for any vascular response. If you can use a spherical lens, it's best to use a silicone hydrogel -- assuming that the lens is available in appropriate prescription powers.
The main concern of post-PK fitting is to minimize trauma to the corneal graft. Contact lenses can cause mechanical and physiological stress that can lead to infection, vascularization or graft rejection. Typically, you'd want to prescribe large diameter (9.5 mm to 12.0 mm) GP lenses to minimize bearing on the graft-host interface and to provide improved stability and centration. A large optic zone size will help to minimize glare.
When fitting the post-PK patient, you'll have the best luck using corneal topography to carefully evaluate the central and peripheral cornea. Waring, et al., and others have developed classifications of post-PK topographies with different GP fitting designs suggested for each (Tripoli, et al.). We see a prolate shape in 31% of post-PK corneas. Aspheric, bi-aspheric or, in cases of a steep graft, keratoconic designs are appropriate for prolate corneas. Another 31% of post-PK corneas have an oblate or plateau pattern.
Because the donor cornea is flatter than the host cornea, it appears sunken. A reverse geometry lens is most suitable for this type of graft. Mixed prolate/oblate corneal shapes (18%) present with a flat side and a steep side with symmetrical astigmatism, which you can correct using a bitoric GP lens. Asymmetrical astigmatism (9%) has been described as a combination of patterns with an irregular or possibly distorted cornea.
One of the most challenging topographies to fit is the "steep-to-flat" pattern (13%). The steep meridian is 180š (from the flat meridian) with an extreme example being graft tilt. Lens centration is difficult, so use large diameter lenses with large optic zone sizes and possibly aspheric curves.
Base the initial GP trial lens base curve on topographic maps, usually the average dioptric value measured 3 mm from the center of the map, or the average keratometry value. Use fluorescein to evaluate the base curve and peripheral curves, with the goal being "divided support" with a balance of one-third touch and two-thirds clearance. A tight lens can lead to lens adherence and compromise the cornea, while flat lenses may cause mechanical injury. Lens centration and position are dependent on the graft shape, and perfect centration is not always possible. Lenses will move in the direction of least mechanical resistance, and lateral displacement is common.
In cases where sutures are present and you can't obtain a successful GP fit because of decentration or mechanical irritation of the sutures, you can use a Softperm (central GP surrounded by a soft contact lens skirt) or a piggyback system (high-Dk GP lens, with a silicone hydrogel underneath) to mask corneal astigmatism, improve lens centration and comfort. You must carefully monitor the Softperm lens, however, as it may become tight-fitting and can easily lead to neovascularization.
OPPORTUNITY ABOUNDS
A wide variety of opportunities exist in which you may fit contact lenses following corneal and refractive surgery. Make sure you wait until the cornea has healed completely, choose the lens that's best for the situation and monitor the patient frequently. Good luck!
References are available on request
Dr. Riley is a faculty member of the Indiana University School of Optometry, where she oversees the Contact Lens Research Clinic and the Contact Lens Residency program. She's a CLEK Study investigator and serves as a research associate in the Borish Center for Ophthalmic Research.
Dr. Silbert is professor of optometry at the Pennsylvania College of Optometry and is director of the Cornea & Specialty Contact Lens Service at The Eye Institute. He is the principal investigator for the NEI-funded multicenter CLEK Study of Keratoconus.
|
HOW TO EARN YOUR FREE CE CREDIT |
|
This Strategic Skill Builders Continuing Education course is made possible by a special grant from Vistakon. To receive COPE-approved credit for this continuing education article, please print and complete the requested information on the official test form which is available as a PDF download. You will need Adobe Acrobat Reader to view a PDF file. You can download it here if you need. Download January 2004 test form Please print out the form, blacken the most appropriate answers, enclose it in an envelope and mail it no later than March 15 to: The Bennett Center Please allow at least six weeks from the closing date to receive your certification. If you pass the test, you'll receive credit from the Irving Bennett Business and Practice Management Center at the Pennsylvania College of Optometry. This course has been approved for continuing education credit by the Council on Optometric Practitioner Education (COPE). The COPE I.D. Number is 10664-CL. |
1. The risk of corneal neovascularization from wearing soft contact lenses is highest after which procedure?
a. LASIK
b. PRK
c. RK
d. LASEK
2. What type of lens best corrects irregular astigmatism?
a. Soft spherical
b. Soft toric
c. GP spherical base curve
d. GP bitoric
3. After myopic LASIK, the corneal shape typically becomes
a. oblate
b. prolate
c. elliptical
d. spherical
4. Reverse geometry lenses . . .
a. usually have large optic zones
b. usually center best with small overall diameters
c. have secondary curves 2.00D to 4.00D steeper than base curves
d. have base curves 2.00D to 4.00D steeper than secondary curves
5. Post-LASIK or post-PRK GP contact lens fits . . .
a. present centration challenges
b. are generally best fit with larger diameters
c. often are best fit with reverse geometry designs
d. all of the above
6. The newer silicone hydrogel lenses with high levels of oxygen transmission greatly reduce the risk of neovascularization.
a. True
b. False
7. Post-surgical complications that benefit from contact lenses include:
a. haloes at night
b. irregularity astigmatism
c. both a & b
d. none of the above
8. With reduced best corrected spectacle acuity caused by posterior keratoconus what type of lens will likely provide the best vision?
a. silicone hydrogel
b. reverse geometry
c. keratoconic design GP
d. bitoric GP
9. Corneal ectasia secondary to LASIK:
a. is usually due to flaps that are too thin
b. shows more irregularity of the posterior cornea than the anterior surface
c. typically can be corrected to as good a VA as in keratoconus fits
d. all of the above
10. Piggyback contact lens fits post-PK:
a. generally allow successful fitting over sutures
b. increase the risk of neovascularization into the graft
c. should use the highest Dk lenses possible
d. all of the above
11. The recommended waiting time post-surgically before fitting contact lenses is longer for PRK than for LASIK.
a. True
b. False
12. GP lenses offer excellent oxygen transmission post PK and can correct astigmatism and smooth out irregular corneal surfaces.
a. True
b. False
13. When corneal surgery results in irregular astigmatism, patients will achieve best possible vision with a GP lens.
a. True
b. False
14. Contact lenses fit before complete, extensive corneal healing after PRK can affect the amount of haze and alter end-point refraction.
a. True
b. False
15. It has been estimated that up to 75% of patients will require contact lenses for best vision post-PK.
a. True
b. False



