CLINICAL
CHALLENGES
The Blurry Teacher
Initial facts didn't point to a clear
answer in this case, but continued testing guided the way.
![]() By
Eric Schmidt, O.D.
By
Eric Schmidt, O.D.
I have said that most of the conditions we encounter as doctors make sense. If we perform detailed examinations and histories and follow them through, then we should arrive at a logical answer as to the cause of a particular patient's problem, condition or disease.
However, cases exist in which even when we "connect the dots" logically, they lead to an unexpected etiology. This is the case in the following patient presentation.
When blurry got blurrier
When I walked into the examination room to evaluate S.K., she smiled at me and said, "I'm either going crazy or I have an eye problem, and I don't know which one would be worse!" She explained to me that for the past 10 days, the vision in her right eye had been blurred throughout parts of the day. She said that when she woke up, the vision was especially blurry, but that it cleared up more or less in about 10 minutes. She described it as if there was "a film" over her right eye. She also noted that at times, colors appeared different and duller through her right eye as compared to her left eye. S.K. said that this was annoying to her at first, but had chalked it up to tiredness until today.
This day, she awoke with the "normal" blurring in the right eye, but it hadn't improved as it usually had. In fact, around 11 a.m., when S.K. was teaching her third grade class, the vision through her right eye became "real blurred." This increase in blurring was enough to bring S.K. into my office for an explanation.
The investigation begins
I asked S.K. some questions in an effort to clarify the depth of her visual loss. She told me that the vision wasn't distorted, just filmy and blurred. She denied any ocular pain and insisted that no problems ever presented with or before the blur. S.K. also explained, after I asked, that there was no pattern to the visual loss. It didn't respect any horizontal or vertical midlines, nor was it consistent in severity each day. She had no associated paresthesia, lightheadedness, headache or any other neurological or systemic symptoms.
S.K. wasn't the typical ocular pathology patient. She was a healthy, 44-year-old, white former Teacher of the Year. She took no medication except for an occasional ibuprofen for "aches and pains." She had no known medical problems, saw her physician regularly and had good eyesight up until this occurred.
As I spoke with her, my mind was spinning with the possible differential diagnoses, but because of her young age and excellent health, my list wasn't comprised of the usual suspects that an eye doctor would think of in other presentations such as this.
|
|
|
|
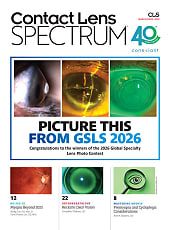
Incipient CRVO. Notice
tortuous veins and swollen optic disc. Also notice the lack of
hemorrhages. |
Taking it one step at a time
The key to a proper diagnosis is to conduct a detailed, step-by-step examination and to try to not prejudice your evaluation with any preconceived notions as to what you think the problem might be. Performing the same exam and then augmenting it with tests that pertain to each particular case will enhance your ability to make the correct diagnosis.
In S.K.'s case, her visual acuity measured 20/25-2 OD, 20/20 OS, but she stated that the left eye appeared to have much clearer vision and that her vision appeared duller with the right eye than with the left eye. Extraocular muscle (EOM) testing showed no restriction of movement and S.K. noted no pain in either eye with this movement. Confrontation fields were full OU, but S.K. said that my face appeared blurry with her right eye but clear with her left eye.
Pupil testing provided me with my first clue: Her pupils measured 6 mm in size OU and were briskly and equally reactive to light. But her right pupil failed to hold the constriction and I graded S.K. as having a 1+ afferent pupil defect (APD).
Following the clues
S.K.'s external examination continued to yield positive results, which helped me hone in on her problem. Amsler grid testing was normal OS, but with the OD, the grid appeared to have a faded yellow hue to it and most of the lines -- both vertical and horizontal -- looked ghosted or doubled.
Color vision testing was normal OU, but there was definite red cap desaturation of the right eye. S.K. told me that the red top was worth $1.00 with her OS and $0.60 with her OD. The slit lamp exam was normal OU, with the exception of mild map-dot-fingerprint dystrophy lesions OU. Specifically there was no rubeosis irides and no anterior chamber cell and flare. IOP was normal at 20 mmHg OD, 18 mmHg OS. S.K.'s blood pressure was measured at 120/78.
Because of the APD, I was certain that there was some optic nerve dysfunction OS. I wasn't expecting to see retinal bleeding, but when I examined her fundus, I saw both retinal bleeding and optic nerve dysfunction. S.K.'s right optic nerve head (ONH) was swollen and erythematous. In addition, scattered dot and flame hemorrhages were evident throughout the posterior pole and the retinal veins were tortuous and dilated inferiorly more so than superiorly (see the image on page 30).
There was no spontaneous venous pulse (SVP) evident OD and it appeared to me that cystoid macular edema was present OD. The retina and ONH of her left eye appeared perfectly normal. There was no disk edema, no macular edema and no retinal hemorrhages. I noted a normal artery-to-vein ratio (A/V ratio) of 2/3 but no SVP.
Getting closer to the answer
S.K. had a unilateral swollen optic disk with retinal hemorrhages and venous caliber changes. My first thought was that she had an optic neuritis (ON), but the absence of ocular pain and the tortuous vessels and macular edema led me to believe that a mild or incipient central retinal vein occlusion (CRVO) may be the diagnosis. (Even though she didn't have any of the typical risk factors for CRVO.)
Because an intravenous fluorescein angiogram (IVFA) is the best way to differentiate between CRVO and ON, I requested one from a retinal specialist. She performed the IVFA and interpreted the results as consistent of a non-ischemic CRVO. There was good capillary perfusion, vasculature tortuosity and multiple dot hemorrhages in four quadrants. The retinal specialist agreed that CRVO was the most likely diagnosis and minimal CME and good perfusion indicated that laser treatment wasn't initially necessary. The retinal surgeon did suggest a complete physical and cardiology workup for S.K. and placed her on 81 mg of aspirin prophylactically. I made this arrangement and specifically requested a coagulopathy work-up from her internist.
Checking progress
In the two months that followed S.K.'s initial examination with me, an internist, a cardiologist, a hematologist and even an oncologist saw her in an attempt to get to the bottom of this presentation. All tests and laboratory work came back essentially normal. And as I said, this patient was an atypical individual to develop a CRVO. All of the healthcare professionals who were involved with her care were concerned that a type of cancer was responsible for her vision problems.
Finally, after much hard work, thinking and investigating, we discovered the reason for the CRVO: S.K. had a Factor V Leiden deficiency, which can lead to hypercoagulation. This could certainly cause a CRVO.
The hematologist prescribed 75 mg clopidogrel and told S.K. to continue taking the aspirin daily. Hopefully, S.K. won't have any further complications either systemically or ocularly because of the relatively early diagnosis.
Reason for relief
I followed S.K. monthly to monitor the CRVO. Three months after her initial presentation, all of the retinal hemorrhages had resolved as did the disc edema. Her visual acuity hovered at 20/25 for six months because of persistent mild macular edema that I noted with a retinal thickness analyzer. I eventually recommended ketorolac tromethamine (Acular) OD q.i.d. in hopes of reducing the CME.
After two months of therapy, S.K.'s macula had returned to a normal thickness, but her visual acuity remains at 20/20-3 OD. She has become much less cognizant of the difference in vision between her two eyes.
Contributing Editor Dr. Schmidt is director of the Bladen Eye Center in Elizabethtown, N.C. E-mail him at schmidtyvision@bellsouth.net.
|
CLINICAL PEARLS |
|