feature
Help for Selecting the Right ICD-9 Codes
for Contact Lens Complications
Clear
definitions for the serious complications will help you choose accurate codes
for easier billing.
By
D.C. Dean, O.D.
When it comes to mastering the science of medical billing for contact lens complications, you need to know how to select the right diagnostic (ICD-9) codes.
We usually have no trouble selecting ICD-9 codes for common complaints because they're listed and defined in the ICD-9 manual. However, several of the more serious conditions, which were named and defined by doctors from abroad, are not listed in the manual, making it difficult for U.S. clinicians to select accurate codes and submit bills for payment.
To help you choose the right ICD-9 codes, I'll translate the foreign terms and definitions into U.S. medical billing terminology so you can select ICD-9 codes for all contact lens complications accurately.
|
|
|
SEAL is characterized by a white lesion in the superior cornea that can be up to 0.5 mm wide and from 1 mm to 5 mm long. |
Common terms
For the most part, you can determine what terms to use for many contact lens complications from the patient history. The ICD-9 codes simply describe symptoms. The top five include:
Blurred Vision – 368.8
Eye Pain – 379.91
Redness of Eyes – 379.93
Dry Eyes – 375.15
Double Vision – 368.2
This list accounts for more than 80% of all contact lens-related complaints, although, we still have to examine the patient's eyes and choose from a number of codes that correspond to our clinical findings.
The two diagnostic codes that stand out, because of their potentially broad application in contact lens practice, include:
Corneal Disorder due to Contact Lens – 371.82
Corneal Edema due to Wearing of Contact Lens – 375.15.
These codes are straightforward.
But that's not the case for the more serious conditions like corneal hypoxia, infiltrates, microbial keratitis and others. These terms are not listed in the ICD-9 manual, which makes it difficult to select the right codes.
To help solve this problem, you can go to www.siliconehydrogels.org, one of the most user-friendly online resources from the University of Waterloo in Canada. It has the most complete glossary of medical terms I've seen.
I'll be using the terms and definitions from this glossary to translate the following contact lens pathologies into U.S. medical language.
CLARE — Contact Lens-induced Acute Red Eye
|
|
|
|
| Patients with corneal microcysts (top) almost always show signs of hypoxia such as corneal neovascularization (bottom) and edema. |
Definition: A sudden onset of a corneal infiltrative event observed during extended wear of hydrogel contact lenses that is always associated with sleep. Patients report waking up with irritation or pain, redness and watery eyes. Sometimes, these symptoms are not noticed until soon after waking. The condition is usually observed unilaterally.
Based on this definition, you should report CLARE symptoms using the following codes:
Eye Pain – 379.91
Redness of Eyes – 379.93
Epiphora – 375.21
Surprisingly, no code exists for corneal infiltrate. To report this diagnosis, choose between one of the following two codes:
Corneal Opacity, Peripheral – 371.02
Corneal Opacity, Central – 371.03
Quite often, patients who have CLARE also have head-cold symptoms. They report fatigue, scratchy throat and runny noses. Others claim to have allergies or hay fever.
These symptoms may be related to viral conjunctivitis — a condition many of us don't think about too often. The ICD-9 code for this condition is 077.99, which is appropriate to use for many CLARE cases. Antibiotic/steroid combination drugs clear up most symptoms of viral conjunctivitis virtually overnight.
CLPU — Contact Lens-induced Peripheral Ulcer
Definition: A circular, well-circumscribed, dense, yellowish-white, focal corneal infiltrate (0.2 mm to 2.0 mm in diameter) located in the peripheral to mid-peripheral cornea. It is always located in the anterior stroma and has a complete loss of overlying epithelium. Symptoms can vary but may include pain or soreness, irritation and watering.
Use the same symptom codes as you would for a CLARE diagnosis. Then, report the clinical findings as follows:
Corneal Opacity, Peripheral – 371.02, or
Corneal Ulcer, Marginal – 370.01
Warning: Don't use the ulcer code unless there is "... a complete loss of overlying epithelium." That's a mistake many nonophthalmologic practitioners make.
Infiltrates are not ulcers. They have an entirely different pathogenesis and treatment protocol.
SEAL — Superior Epithelial Arcuate Lesion
Definition: Thin arcuate white lesion in the superior cornea, within 1 mm to 3 mm of the superior limbus between 10 and 2 o'clock. SEALs can be up to 0.5 mm wide and from 1 mm to 5 mm long, sometimes with heaped edges. Diffuse infiltration underlying the lesion is possible.
The critical finding that defines SEALs is the presence of the peripheral white lesion, which should be obvious even without the use of vital stains.
To code this condition, use Corneal Opacity, Peripheral – 371.02. Many clinicians have reported complete resolution of this complication by simply switching the patient to a lower modulus lens material.
|
|
|
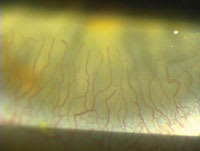
Corneal ghost vessels, the most common diagnosis of hypoxic stress, is best treated with the highest tolerable Dk hydrogel lens. |
Microcysts
Definition: Small (15 μm to 50 μm), irregularly shaped inclusions, usually found in the paracentral to mid-peripheral zones of the cornea. Observation is best with retro-illumination. Microcysts show reversed illumination due to a suspected higher refractive index than the surrounding tissue. A hypoxic mechanism has been proposed for microcyst development, involving a reduced epithelial mitotic rate and slower regeneration of the epithelium.
Since microcysts are clear, using the corneal opacity codes wouldn't be appropriate. What's more, patients with microcysts rarely report symptoms. So it seems as though we wouldn't be able to describe the condition with existing ICD-9 codes.
But if you look at the underlying cause of this condition, you'll notice these patients have significant corneal hypoxia. It's possible there may be patients with microcysts who don't have other clinical signs of hypoxia, but I've never seen them in my practice. So if you re-examine these corneas, you'll almost always see these related hypoxic pathologies:
Corneal Edema, CL induced – 371.24
Corneal Neovascularization – 370.60
All medical visits, including the 92000 level ophthalmologic specialty codes, require a treatment plan related to an ICD-9 diagnosis. The obvious treatment for patients suffering from hypoxic corneas due to low-Dk HEMA lenses is to immediately refit them for the highest tolerable Dk silicone hydrogel lens. Reason: These patients don't want to wear eyeglasses and, therefore, are likely to continue wearing their old lenses if you don't refit them right away.
A growing number of patients new to my office, who are currently wearing a silicone hydrogel lens, show clear signs of previous hypoxic corneal stress they've had from years of low-Dk lens wear. The most common diagnosis seen in these patients:
Corneal Ghost Vessels – 370.64
|
|
|
You can treat contact lens-induced papillary conjunctivitis, also known as giant papillary conjunctivitis (GPC) with modern silicone hydrogel lenses. |
The proper treatment involves an immediate refit for the highest tolerable Dk silicone hydrogel lens. Dr. Charles Edmonds has conducted some excellent clinical studies that show how traumatized the corneal endothelium becomes under low-Dk HEMA contact lenses. For this reason, I include a statement on each chart, advising the patient to avoid all HEMA contact-lens wear in the future.
CLPC — Contact Lens-induced Papillary Conjunctivitis
Definition: Symptoms may range from mild hyperemia of the upper tarsal conjunctiva with a few, small papillae to severe hyperemia with large, raised papillae, which have a cobblestone appearance. CLPC may present as a localized or generalized response. Symptoms include itching and a stringy or ropy mucous discharge. Excessive lens movement or decentration and blurred vision may also occur. Lens material, design or fitting characteristics may need to be modified to prevent recurrence of this condition.
Most of us would recognize this complication as Giant Papillary Conjunctivitis (GPC), a condition so common you'd expect it to have a code listed in the ICD-9 manual. A code does exist, but it's not called GPC. It all depends on the etiology. Since papillae aren't follicles, we can't use the code for follicular conjunctivitis. If the underlying cause is allergic, then the appropriate code would be:
Chronic Allergic Conjunctivitis – 372.14
The definition of CLPC, however, says contact lenses cause the condition. The treatment involves modifying the contact lens parameters, not using antihistamines. So the proper code to report CLPC should be:
Chronic Conjunctivitis, unspecified – 372.10
Proposed etiologies for CLPC include mechanical abrasion from poor edge design and protein film abrasiveness. Modern silicone hydrogel lens designs address both problems and, therefore, are the logical choice for a treatment option.
|
|
|
Microbial keratitis (MK), caused by bacterial, viral, fungal and amoebae organisms, also can be treated with high-Dk silicone hydrogel contact lenses. |
MK — Microbial Keratitis
Definition: Microbial keratitis occurs as a result of an infection of the cornea by replicating microbes (bacterial, viral, fungal or amoebae). In contact lens wear, it is usually preceded by hypoxia and/or an epithelial break. Contact lens wearers (particularly extended wear) are more prone to develop MK. The most common microbe associated with contact lens-related MK is a bacteria called Pseudomonas aeruginosa.
Researchers have found that bacteria tend to bind to the back surface of silicone hydrogel lenses after patients have been swimming. For this reason, I always recommend patients remove and disinfect their lenses after any exposure to pools, lakes or rivers.
Symptoms of MK include rapidly increasing pain, severe redness, intense epiphora and photophobia. Paracentral or central lesions can have full thickness loss, raised edges and an irregular appearance. Anterior chamber flare also may be present.
Here's a list of ICD-9 codes you can use to report MK:
Corneal Ulcer, Central – 370.03
Secondary Iridocyclitis, Infectious – 364.03
Eye Pain – 379.91
Epiphora – 375.21
Redness
of Eyes – 379.93
Photophobia – 368.13
Keep in mind ICD-9 coding allows you to report a condition, such as corneal ulcer, without having to document the symptoms related to the underlying pathology.
I wouldn't report any of the last four codes in the above list if I were billing for this patient, since they refer to symptoms directly related to the clinical findings, and I'd be addressing them in treatment.
So why do these potentially sight-threatening conditions occur? Notice that the definition of MK contains a key clue, "... it is usually preceded by hypoxia and/or an epithelial break." Most physicians are aware that patients wearing silicone hydrogel lenses also can develop MK, but you want to reduce the odds as much as possible. The higher-Dk lenses have virtually eliminated hypoxia. And their nonionic surface characteristics have almost eradicated abrasive protein film deposits. Thus, fitting every appropriate patient into a high-Dk lens should prophylactically prevent conditions likely to cause MK.
Unlike MK and the other conditions just mentioned, the definitions of the following contact lens complications are actually listed in the ICD-9 manual, and, therefore, are easier to code.
SPK — Superficial Punctate Keratitis
ICD-9 allows you to report punctate keratitis as 370.21 or superficial keratitis as 370.20. The definition in the ICD-9 manual shows the code 370.21 is for Thygeson's SPK, which includes the finding of keratic precipitates after injury or iridocyclitis. So the appropriate code to use for contact lens-related SPK is 370.20.
Exposure Keratitis
The term exposure keratitis can't be found in the ICD-9 manual. The proper terminology is Exposure Keratoconjunctivitis (370.34), defined as, "Incomplete closure of eyelid causing dry, inflamed eye." It's best treated with the use of a therapeutic contact lens (92070) that can stay on the eye safely overnight and protect the cornea from dessication. Currently, the only silicone hydrogel lens approved for this purpose is CIBA Night & Day.
Keratoconjunctivitis Sicca
Coding for keratoconjunctivitis sicca is not as straightforward as it may first appear. The condition involves reporting biomicroscopic findings without referring to the underlying cause. You shouldn't use the code 710.20 if your patient suffers from Sjögren's syndrome.
Yet, if a lacrimal gland insufficiency is found through clinical testing, you can use the code 375.15 for tear film insufficiency. The ICD-9 definition for keratoconjunctivitis sicca states, "...decreased flow of lacrimal (tear) is a contributing factor." However, it's best to use the code 370.33 to report keratoconjunctivitis sicca before performing more specialized tests for lacrimal gland function. This code indicates you're simply reporting what you see through the biomicroscope before performing more tests.
You can make ICD-9 coding easier for you and your billing staff if the codes I've discussed are listed on your fee slips. You'll save time and aggravation since no one will have to look up these codes on a busy clinic day.
Just as a reminder, insurance companies aren't concerned about the clinical logic of practitioners. They publish specific medical policies that each contracted physician should read and apply to treatment and billing protocols.
Unfortunately, most of us older O.D.s have never had medical-billing course work in school, so it's important to regularly attend educational meetings with local and state optometry organizations to discuss proper coding and billing procedures. You'll reap substantial professional, personal and financial rewards from a well-run medical billing practice.