High-tech scanning laser ophthalmoscopy imaging devices ensure you’re providing your retinal disease patients with the best care possible.
Currently, most optometrists rely on standard direct and indirect ophthalmoscopy to view the retina. Although we can detect much retinal pathology this way, retinal imaging devices allow for either greater field-of-view (as with Panoramic scanning laser ophthalmoscopy) or greater depth-of-view (as with optical coherence tomography, or OCT, and devices that analyze retinal thickness). These greater views decrease our likelihood of missing signs of retinal disease and aid in early disease detection, diagnosis and management.
While retinal imaging devices are currently considered stateof- the-art, someday soon, they may become standard-of-care. For this reason, you should be aware of the clinical applications of these devices, their principles of operation, how you can incorporate them into your practice and the coding and billing involved in employing them. Here, I cover all these topics.
Clinical applications
Retinal-imaging devices have three main clinical applications: 1. Pathology detection in the far peripheral retina. The Panoramic scanning laser ophthalmoscopy device, from Optos, is an adjunctive technology to binocular indirect ophthalmoscopy (BIO), as it enables you to detect structural abnormalities, such as tears, holes, tumors and vascular anomalies, that you might miss with BIO alone.
It provides a 200° view of the retina in any one image. This is often enough to view the entire posterior pole and much of the retinal periphery.
In contrast, BIO provides a 30° view in any one image, using a standard 20.00D lens. In the periphery, you can often see a sliver or partial view of the retina at any one time, requiring you to view multiple areas of the retina to get a complete view — something that is both time-consuming and uncomfortable for the patient.
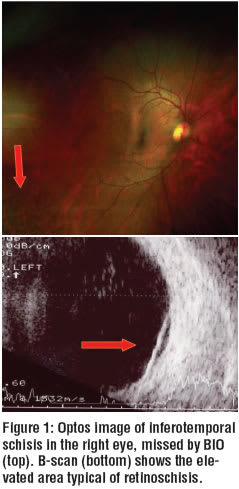
You can see the clinical benefit of this particular device in a 54 year-old female who was referred for evaluation of a superotemporal retinoschisis in her left eye. Her primary optometrist discovered this during a dilated fundus examination of both eyes with BIO.
Imaging with the Panoramic 200 revealed a larger, but flatter inferotemporal retinoschisis in the patient’s right eye. This was missed by BIO on previous examinations (see figure 1).
Something else to keep in mind: The Panoramic 200 also allows you to measure the size of lesions. This is important for monitoring change over time, as in tracking a choroidal nevus. Also, you can use this device to view the peripheral retina when patients can’t or don’t want to have their pupils dilated. This provides an extra dimension of care and convenience for these patients.
2. Detection of in-depth structural abnormalities beneath the retinal surface not apparent with BIO. OCT devices are useful when the cause of a patient’s visual complaint isn’t obvious via BIO. This is because the OCT performs a cross-sectional analysis of the retina, allowing you to view abnormalities beneath the retinal surface.
For example, a patient complaining of mild blurry vision when reading presented with folds in her macula (see figure 2). The reason for the folds wasn’t immediately clear. So, I employed the OCT. The line scan of the device revealed the presence of vitreo- macular traction syndrome. As a result, we were able to determine that the photo-receptor layer was still intact, though stretched. Because her visual acuity was 20/25, we determined the best course of action was to monitor the patient, as opposed to surgical intervention.
3. Diagnosis of abnormalities causing retinal thickening or thinning. Retinal-imaging technologies, such as OCT and devices that analyze retinal thickness, enable you to view into the depth (sort of an “in-vivo” dissection) of the retina to confirm and quantify retinal thickening or excavation. Once you obtain these values, you can then compare them against an age-related normative database, as with visual field testing to determine whether the retinal thickness or thinning is outside normal limits. This can help you determine the diagnosis and initiate appropriate treatment.
BIO can appreciate to some extent the changes in retinal depth, but it can’t quantify these changes.
Principles of operation
Each retinal-imaging device uses a different principle to image the retina. The eye-care market offers several excellent retinal- imaging devices, including those described below and listed in the sidebar on page 43.
• Panoramic 200 Scanning Laser Ophthalmoscopy (Optos). This instrument has a scanning device, which uses different frequency lasers and an ellipsoidal mirror to gather information from multiple layers of the fundus. The green laser (532nm) captures information mainly from the neurosensory retina to the retinal pigment epithelium (RPE), whereas the red laser (633nm) captures information from the pigment epithelium posterior into the choroid; however, there is some overlap.
The device simultaneously obtains and makes available both green and red separation

views (in addition to the composite view). But if necessary, subtle retinal findings, such as retinal hemorrhages, are most obvious with the “green separation” view, and subtle findings at the level of choroid, such as a choroidal nevus, are most obvious with the “red separation” view. This allows for differential diagnoses of most lesions within the view of this instrument. It takes only three to five minutes to complete an exam for both eyes.
•Stratus OCT (Carl Zeiss Meditec). This device utilizes an ~800nm laser that employs the principle of backscattered light to provide a two-dimensional cross-section of the retina with a resolution of 10 microns. OCT imaging measures the echo-time delay and intensity of backscattered light. Each layer of the retina has different backscattering properties and appears as a different color on the display (a “false-color” scale).
For example, the retinal nerve fiber layer and the retinal pigment epithelium have the greatest backscattering properties and appear in red on the display. Other layers, such as the inner retina and photoreceptors, have less backscattering properties and appear as green and blue colors respectively. Features, such as fluid-filled spaces, appear as black, hypo-reflective pockets.
OCT is like ultrasonography, except the instrument uses light instead of sound, and the resolution of tissue layers is much greater.
The Cirrus High-definition (HD)-OCT (Carl Zeiss Meditec) uses a different technology — spectral, or Fourier domain, technology — to capture volumetric (3-D) and high-definition line scans of the retina. It has FDA clearance and should be commercially available this fall.

• RTA 5 (Marco). This instrument utilizes a vertical, narrow, green helium-neon (HeNe) laser (543.3nm) to project a slit-beam at an angle, while a charge-coupled device (CCD) camera records backscattered light. The backscattered light is reflected off the vitreoretinal internal limiting membrane and chorioretinal RPE surfaces.
The RTA obtains a 3mm X 3mm scan consisting of 16 optical cross-sections across the posterior pole at nine different positions. The device then uses the thickness of each slit to construct a three-dimensional image or retinal map. The resulting 3-D map depicts areas of retinal thickening or retinal thinning as with the case in figure 3.
•Heidelberg Retinal Tomography (HRT). This instrument takes topographic images of the optic nerve head. Through the HRT Retina mapping program, you can apply this same
Coding and billing
The following classes of retinal disease support medical necessity
of diagnostic imaging (CMS breaks them down further by
ICD-9 CM code). It’s not enough to link the procedure code to
the appropriate diagnostic code. The diagnosis or clinical signs
and/or symptoms must also be present.
a) retinal tumors and cysts
b) retinal detachment
c) retinoschisis
d) retinal tear; retinal hole
e) multiple defects of retina without detachment
f) diabetic retinopathy (all stages)
g) macular edema
h) macular hole
i) macular pucker
j) hypertensive retinopathy
k) exudative retinopathy
l) vascular changes
m) vascular occlusive diseases
n) central serous choroidopathy
o) serous detachment of the RPE
p) macular degeneration (all forms)
q) toxic maculopathy
r) vitreoretinal degenerations and dystrophies
s) retinal dystrophies
t) retinitis
u) choroiditis
v) choroidal degeneration
w) pars planitis
technology to imaging the macula. With the Retina mapping program, the HRT utilizes a scanning laser ophthalmoscope to take three sets of 32 images with thousands of height measurements of the fundus, as it does with the optic nerve, from an anterior to a posterior plane, perpendicular to the optical axis.
A computer software program then aligns the images and compiles a three-dimensional image of the scanned surface. Clinically, the program detects changes in macular thickness.
•Spectralis (Heidelberg). This recent addition to the OCT market performs simultaneous OCT imaging and fluorescein angiography using the Heidelberg Retina Angiograph (HRA), which provides high-speed, highresolution OCT.
A patient presented with wet age-related macular degeneration (AMD) and had an occult choroidal neovascular membrane below the RPE, which was therefore not directly visible via BIO (see figure 4). Angiography (using either fluorescein or indocyanine green dye) is crucial in detecting these types of membranes, but the simultaneous OCT image provides a real-time, in-vivo localization of the choroidal neovascular membrane. This is important because you can now see the extent of the lesion beneath the retina.
The Spectralis is also capable of performing fundus “autofluorescence,” a technology that is gaining popularity in the detection and progression of AMD through the monitoring of lipofuscin concentrations.

• RTVue-100 (Optovue, Inc). This high-speed, high-resolution OCT is the first FDA-cleared Fourier-domain OCT (FD-OCT). [The Stratus OCT is considered time domain (TD); Spectralis and Cirrus HD-OCT, both FDAcleared, are Fourier domain (FD), also known as Spectral domain (SD)]. FD-OCT, or SDOCT, collects an entire A-scan at once, instead of sequentially (like TD OCT), so that in 0.04 seconds, the device collects 1,024 A-scans. FD-OCT, or SD-OCT, collects more data in less time than TD-OCT.
Because it collects data faster than eye movements, the images are not subject to variability from patient’s eye movements. It also collects twice the amount of data within this period of time, resulting in a higher-resolution image (5 microns) than with standard TD-OCT.
Higher resolution allows for more precise detail, which allows for a better understanding of the histology of retinal disease. The device also allows for 3-D imaging, which is superimposed above the A-scans for better localization of pathology. However, it remains to be seen whether the higher resolution affects clinical diagnosis and management (see figure 5).
Incorporating retinal imaging into your practice
The decision to purchase or to enter into a user agreement for a retinal-imaging device depends on your patient base, the space available in your practice and your finances. While some of you may not have the patient base for these instruments, you may still want to offer an additional level of care that separates you from other eye-care practitioners. (See “SLO Retinal Imaging Device Manufacturers,” page 43.)
So, how much will you invest to acquire one of these devices?

With the exception of the Optos, which you cannot purchase, the cost of these devices is upwards of $60,000 and more for the high-speed, high-resolution devices. (While you can’t purchase a Panoramic 200, you can enter into a user agreement with the company using a variety of options.)
If you decide to purchase one of these devices, the manufacturer will send a representative to train someone from your staff on how to operate the chosen device (image speed and quality of image acquisition improve with experience).
Some helpful additional information:

• For imaging of the retina, the Panoramic 200 doesn’t require pupil dilation, so a staff member can obtain an image in addition to other initial auxiliary testing. And, because it doesn’t require pupil dilation, patients appreciate that they don’t necessarily need to be dilated at each exam.
• For all retinal mapping technologies (OCT and RTA, Heidelberg Retinal Mapping program), it’s best to dilate the pupil. OCT imaging takes about five to 10 minutes, depending on the patient. RTA takes about 15 to 20 minutes. The Heidelberg Retinal Mapping Program and Spectralis OCT also require pupil dilation for best quality images. The former takes about five to 10 minutes and the latter may take more time due to simultaneous flourescein angiography.
• The RTA takes about 15 to 20 minutes (depending on the version) to perform its exam. You should be aware of two codes for retinal imaging devices:
• 92135. Use this CPT/ HCPCS code for OCT and RTA technology. It represents scanning computerized ophthalmic diagnostic imaging (e.g., scanning laser) with interpretation and report; unilateral.
If you need to scan both eyes, you must use a “50” modifier. If you refer a patient to another facility for the technical portion of the testing, but you wish to provide the interpretation with report, you can still bill for the procedure using a “26” modifier (in addition to the “50 modifier” if you’re scanning both eyes). Remember, however, to notify the facility performing the imaging that you’ll be billing for the interpretation component and they will bill for the technical component, which requires a “TC” modifier.
CMS will reimburse 60% of the technical portion of the examination and 40% for the professional or interpretation component.
You may bill your component separately or in conjunction with the usual E/M codes if the patient is returning to your office.
• 92250. Use this code (fundus photography) for the Panoramic 200 if the patient has pathology. If, however, you’re using this device as an adjunctive test for screening purposes, let the patient know that he is responsible for payment. (Typically, doctors charge around $40 for the procedure if it’s being used for screening purposes. Often, patients are willing to pay this fee for the convenience of not having to be dilated and getting a full evaluation of their retina.)
Because retinal imaging devices aid in the detection, diagnosis and management of retinal disease patients, you should consider purchasing or using one if you follow such patients.
They lessen the likelihood that you’ll miss disease and demonstrate to your patients that you are aware of-, and well-versed in, the latest technology and thus providing them with the most thorough care possible.
Yes, these devices are currently state-of-the-art, but it won’t be long before they become standard-of-care. Will you be ready?

Dr. Bass is a distinguished teaching professor at the State University of New York (SUNY) State College of Optometry. She lectures extensively in retinal disease and teaches in the retinal clinic. E-mail her at sbass@sunyopt.edu.



