update on surgery
NEW TECHNOLOGY IOLS: New Rules
By being aware of these eight issues, you have an excellent chance of creating happy postoperative patients.
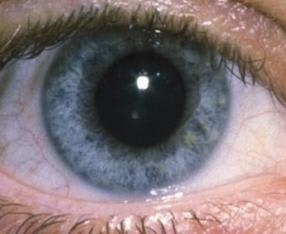
For the patient to achieve success with a multifocal IOL, his pupil must be able to dilate in dim light and constrict in bright light.
J. JAMES THIMONS, O.D., Fairfield, Conn., and CHRISTOPHER J. QUINN, O.D., Iselin, N.J.
With new technology comes a new set of rules for how we practice. This is particularly the case with the premium intraocular lens (IOL) offerings: accommodative and multifocal lens designs.
While researchers are publishing a remarkable amount of material on these new systems, the majority is related to the technical considerations of lens design and surgical approach. (See "Roadmap for IOL Success,".)
Although this information is important in the overview of these systems, it's just as critical for you to have an understanding of the practical side of the process. The fact is, while these systems can provide excellent vision to your cataract patients, you must be aware of the issues surrounding these lenses to ensure patient satisfaction.
Here, we discuss these issues.
1. RESIDUAL AMETROPIA
The optics of the multifocal IOLs create a difference in patient response relative to the level of refractive error. The reason for this is that even small residual refractive errors can produce significant patient concerns about best visual function.
As a result, it's imperative you perform accurate preoperative biometry and use a nomogram, such as the clinical history method, that's been most successful for the multifocal in which the ametropic patient is interested. Doing these things minimizes the risk of even a small "refractive miss."
Should residual astigmatism be a problem post-multifocal implantation, the surgeon can often perform astigmatic keratometry.
2. ABERROPIA
In 2002, ophthalmologist Amar Agarwal, of India, coined the term aberropia to identify patients whose vision loss is exclusively due to higher-order aberrations and not refractive power.
In the case of premium IOL implantation, aberropia can prevent patients from obtaining optimal vision from their lenses.
As a result, you may want to employ an aberrometer on these patients prior to cataract surgery. Once you correct these aberrations, via refractive surgery, many of these patients can regain their normal vision and thus receive the full benefits of their IOLs.
| Aberropia, which is vision loss due exclusively to higher-order aberrations and not refractive power, can prevent patients from obtaining optimal vision from their lenses. |
3. POST-REFRACTIVE SURGERY CORNEAS
When a patient undergoes refractive surgery, the shape and length of his cornea changes, making pre-refractive surgery readings of the cornea's curvature obsolete.
As a result, when these patients present for either accommodative or multifocal IOL implantation, you must carefully calculate the patient's corneal refractive power. Do this by using a nomogram to ensure the patient's IOL has the appropriate power.
4. OCULAR CONDITIONS
Multifocal IOLs may further decrease contrast sensitivity in patients who already have compromised visual function. This is theoretically possible, as the separation of distance and near performance in these IOLs is at the expense of contrast quality in certain situations.
An example: If you place a new multifocal IOL in a patient who has age-related macular degeneration (AMD), or someone who has posterior capsular opacification (PCO), and that patient drives in either bright sunlight or meets oncoming headlights at night, the patient is most likely going to experience distortion, glare and scattering halos. This is because the multifocal lens may add a contrast loss on top of the existing loss, which can actually amplify the patient's visual problems.
In the case of PCO, it is interesting to note that the level of opacification is non-linear to visual function, and the magnitude of the visual enhancement is frequently much greater than the level of opacification indicates.
| Because multifocal IOLs require maximal visual pathway performance to provide the best vision, consider referring patients who have existing contract loss for a YAG laser capsulotomy. |
Because multifocal IOLs require maximal visual pathway performance to provide the best vision, you may want to consider referring these patients for a Yttrium Aluminum Garnet (YAG) laser capsulotomy.
5. PUPIL DYNAMICS IS IMPORTANT
In selecting a multifocal IOL, pupil dynamics are critical to maximize lens performance. This is because both the apodized system and the zonal system operate under different optical principles.
Therefore, in order for the patient to achieve maximum success with the apodized lens system, the pupil must be able to dilate in dim light and constrict in bright light. Not all patients can achieve this. In general, pupillary function declines with age.
6. NEURAL ADAPTATION
The success of multifocal IOL implantation is contingent on neural adaptation. This is the re-teaching of the visual system to select between two separate and distinct images. We have found that neural adaptation can take as little as a day or as long as six months.
7. MONOVISION
One of the current trends in accommodative IOLs is to mix the lens systems to create a "New Millennium" monovision. Unlike past monovision techniques in contact-lens wear and laser surgery, the rules involving monovision via these IOLs are still evolving. As a result, there is currently an absence of peer-reviewed material to instruct us on the best way to go about this.
Although various surgeons have reported great success in choosing the higher power add for near in the dominant eye and the lower add power lens for distance in the non-dominant eye, others have chosen the opposite route. Since this is not yet an exact science, we must often work with these patients until they achieve their desired outcome.
8. HIGHER REIMBURSEMENT
Due to the aforementioned issues, premium IOLs require a significantly greater level of pre- and post-operative care than what is required with monofocal IOLs.
Medicare compensates you, the comanaging clinician, for your services at a rate of 20% of the global surgical fee for cataract extraction with a monofocal lens. With premium IOLs (considered a non-covered service by most payers), the free market determines the cost to the patient. This cost includes the price of the lens as well as the professional services both you and the surgeon provide.
Premium IOLs boast a higher price tag, (they can cost as much as $2,500 to $3,000 per eye and more than not, are not covered by insurance). In addition, practitioners are heavily marketing these system's technological advancements, such as these lenses' ability to be matched with patient lifestyles. As a result of these developments, the current cataract and refractive surgery patient has a higher level of expectation relative to visual performance, than the monofocal IOL patient.
To ensure your patient's expectations do not differ from your own, discuss all the aforementioned issues relative to each patient prior to their decision to undergo multifocal implantation. Remember: A surprised patient is an unhappy patient. OM

Dr. Thimons is a national and international speaker on eye care and serves as medical director at Ophthalmic Consultants, in Fairfield, Conn. E-mail him at jthimons@sbcglobal.net. |

Dr. Quinn is center director of Omni Eye Services, a regional optometric comanagement center with offices in New Jersey. E-mail him at quinn@omnieyeservices.com. |



