comanagement
Comanaging Vitreo/Retinal Disorders
The following three items should comprise the solid foundation for caring for these patients.
Larry J. Alexander, O.D., F.A.A.O., McKinney, Texas
Although the comanagement protocol for patients who have vitreo/retinal disorders has been debated, there remains no solid foundation for the comanagement of these patients. In other words, no identifiable written-guidelines concerning these patients exists.1 In order for both the patient and the primary-care doctor to achieve successful outcomes, I believe the following three items should comprise the comanagement protocol concerning patients who have vitreo/retinal disorders:
1. Knowledge of clinical anatomy
In order to effectively diagnose and comanage a patient who has a vitreo/retinal disorder, the primary-care optometrist must understand clinical anatomy, alteration of that clinical anatomy and the implications of that alteration.
An example: The presence of intraretinal edema and the proximity of that edema to the foveal avascular zone. With newer techniques for managing this type of situation, such as anti-VEGF therapy, coupled with early intervention resulting in optimum outcomes, it is incumbent on the primary-care optometrist to recognize this, among other anatomical changes.2-8
Possessing such knowledge enables the primary-care optometrist to know when to hold the patient and when to ask for a consult. Over-referral is not productive, but timely consultation is productive.

This photo shows retinal pigment epithelial disease with probable underlying choroidal disease. The process is creating outer retinal edema lifting both the RPE and the neurosensory retina. Without knowledge of clinical anatomy, alteration of that clinical anatomy and the implications of that alteration, the primary-care O.D. cannot effectively diagnose nor comanage patients who have vitreo/retinal disorders.
2. The right tools
The proper clinical tools will assist the primary-care optometrist in understanding underlying clinical disease and applying timely consult requests. With that said, realize that you cannot diagnose and comanage what you cannot see. In their early stages, virtually all posterior pole vitreo/retinal disease is not observable without time- or spectral domain technology. (A partial list of posterior pole vitreo/retinal disorders that are difficult if not impossible to visualize in their early or subtle stages with standard techniques, such as ophthalmoscopy and fundus lens examination, are represented in Table 1.) If the primary-care optometrist has the diagnostic tools to effect early diagnosis, those very same tools can enable the effective follow-up of that patient within the realm of comanagement.
Table 1. Difficult to Visualize

Additionally, concerns exist regarding retinal issues outside the posterior pole, such as a retinal break and small peripheral malignancy. Early intervention results in better outcomes in these issues as well. To identify and comanage peripheral retinal disorders, however, you must utilize peripheral viewing technology in the form of routine binocular indirect ophthalmoscopy and/or wide-view imaging technology.
While from an epidemiological standpoint the posterior pole presents problems more frequently, issues in the peripheral retina do create significant threats to vision, so it's essential to look for these conditions as well.

This photo shows spectral domain imaging of change analysis regarding diabetic macular edema pre- and post-anti-VEGF injection. This management of change analysis is critical in the comanagement arena.
3. A comanagement contract
Now, armed with a good understanding of applied clinical anatomy and physiology and the right tools for diagnosis and comanagement, the primary-care optometrist must meet with the retinal specialist and develop a specific protocol regarding the specialist's provision of care and the comanagement of care.
A written protocol, or algorithms, ensure compliance with a number of issues including: (1) the best interest of the patient, (2) proper pre-appointed follow-up, and most importantly (3) a formal two-way communication between the primary-care optometrist and the retinal specialist, which is a mandate of Medicare payment and legal guidelines.
While every patient is unique and every intervention must be tailored to the patient, certain general guidelines can be elucidated and followed. These guidelines must be “plastic” and routinely modified based on the evolution of “new” diagnostic techniques and intervention. (See “Comanagement Algorithm for Branch Retinal Vein Occlusion,” below.)
The cornerstone of all comanagement is communication between the primary-care optometrist and the retinal specialist. This communication must be maintained throughout the care of the patient and must be appropriately documented in the chart of both healthcare providers. Remember as well that guidelines dictate that there must be a written transfer agreement between the specialist and the primary provider.9 This is so the primary-care optometrist can get reimbursed for his services, and it's a general rule.

Here's an example of a peripheral retinal disorder that would have been difficult to find without either a dilated binocular ophthalmoscopic examination or wide-field imaging.
Without a solid foundation for the comanagement of vitreo/retinal disorders, we may miss these conditions, placing our patients at risk for vision loss, and/or we may lose these patients to other eyecare practitioners. By following the aforementioned comanagement protocol, however, I believe primary-care optometrists have an excellent chance of achieving successful outcomes for both their patients and practice. OM
I challenge the professions to develop and publish a basic management protocol by way of consensus panels to assure improved patient care and better efficiencies within the healthcare system.
1. Bucar AA. Intraprofessional consultation and comanagement. Optometry. 2008 Feb;79(2):61-2.
2. Lowenstein A. The significance of early detection of age-related macular degeneration: Richard & Hinda Rosenthal Foundation Lecture, The Macula Society 29th annual meeting. Retina. Sep27(7): 873-8.
3. Arias L, Armada F, Donate J et al. Delay in treating age-related macular degeneration in Spain is associated with progressive vision loss. Eye (Lond.) 2009 Feb;23:326-333.
4. Boyer D, Antoszyk A, Awh C, et al. Subgroup Analysis of the MARINA Study of ranibizumab in neovascular age-related macular degeneration. Ophthalmology. 2007 Feb;114(2):246-52.
5. Maguire MG, Alexander J, Fine SL; Complications of Age-related Macular Degeneration Prevention Trial (CAPT) Research Group. Characteristics of choroidal neovascularization in the complications of age-related macular degeneration prevention trial. Ophthalmology 2008 Sep;115(9):1468-73.
6. Nguyen QD, Shah SM, Heier JS, et al. Primary End Point (Six Months) Results of the Ranibizumab for Edema of the macula in Diabetes (READ-2) Study. Ophthalmology 2009 Nov;116(11):2175-81.
7. Diabetic Retinopathy Clinical Research Network, Elman MJ, Aiello LP, et al. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 2010 Jun;117(6):1064-1077.
8. Gündüz K, Bakri SJ. Management of proliferative diabetic retinopathy. Compr Ophthalmol Update. 2007 Sep-Oct;8(5):245-56.
9. Corcoran Consulting Group. Co-Management of Postoperative Care. January 2008. www.corcoranccg.com/GetFile.aspx?FileID=42e3f0db-4319-491e-9dc7-a71c8e9818c0 (Accessed May 18, 2011.)
| Comanagement Algorithm for Branch Retinal Vein Occlusion |
|---|
| Retinal Vein Occlusion is a relatively common cause of vision compromise associated with the possibility of macular edema and retinal ischemia. I've found that branch vein occlusion is three times more common than central vein occlusion with both more common in patients age 60 and older. Ocular ischemic syndrome may present as a variant of central retinal vein occlusion, and internal carotid disease must be considered in the diagnosis. Symptoms of branch retinal vein occlusion are largely dependent on the location of the occlusion and the subsequent impact on macular function. Neovascularization of the retina and optic nerve may occur with ischemia. Elevated intraocular pressure may also have an association with vein occlusions. The following algorithm may be altered based on the primary-care optometrist's discussion with the retinal specialist and his or her comfort level. 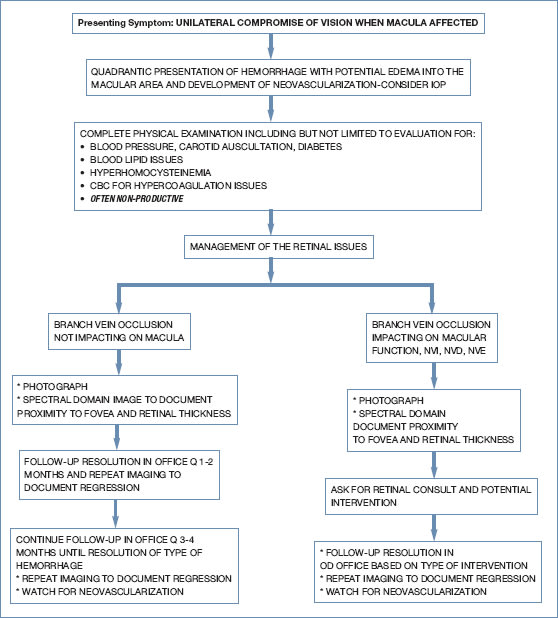
|
| Dr. Alexander is the senior director of Clinical Education for Optovue, Inc. In addition, he's president of the Optometric Retina Society and a member of the Medical Advisory Board for the Macular Degeneration Association. E-mail him at larryalexander@tx.rr.com, or send comments to optometricmanagement@gmail.com. |



