The Medical Economics of Dry Eye
Create new revenue streams by doing more for your patients
■ By Doug Devries, OD
There are many good reasons to develop a strong dry eye component within your optometric practice: your patients’ well-being, their perception of you and your practice, the prevention of contact lens dropout, and the referrals that come from treating this chronic, progressive disease. Don’t forget, too, that it can help with the financial health of your practice, which is under attack from many angles, including online dispensaries and decreasing vision plan reimbursement.
You really only have two choices for protecting your revenue stream. You can either see more patients or you can do more for the patients you already have.
Dry eye is a great opportunity to do more — to provide much-needed services for your existing patients. Millions of people suffer from dry eye, including millions of baby boomers, a large percentage of whom are post-menopausal females, who are now joining Medicare, and the majority of eye exams are performed by optometrists. All of this points to the fact that dry eye patients are already in your practice.
In our practice, we’ve created several dry eye-related revenue streams to help us treat our patients, and you can do the same.
Testing and Documentation
The availability of point-of-care testing for dry eye is a positive development. Two notable testing options have been making their way into an increasing number of practices: the TearLab Osmolarity System and InflammaDry (RPS). Technicians can perform either of these tests efficiently as part of the patient workup, and both companies help with training, practice logistics, marketing, and every other aspect of adoption.
For Medicare patients, testing with InflammaDry (CPT code 83516) and the TearLab Osmolarity System (CPT code 83861), both considered in vitro laboratory devices, is billed under the Clinical Laboratory Fee Schedule, not the Physician Fee Schedule. Therefore, Medicare patient co-payments or deductibles don’t apply; the service is 100% reimbursed. (Coding requirements for commercial carriers may vary.) Optometrists should embrace point-of-care testing as a means to achieve more accurate diagnoses. Not doing so might mean exclusion from insurance panels. Both InflammaDry and the osmolarity test require a practice to have a Clinical Laboratory Improvement Amendments (CLIA) waiver, which isn’t difficult to obtain in the vast majority of states.
In addition to point-of-care tests, standard meibography and anterior segment imaging, including new features on some topographers and tomographers, can be used to help detect and document the signs and causes of dry eye. The LipiView interferometer (TearScience) takes meibography to a new level with its abilities to measure lipid layer thickness, evaluate blink rate, and allow visualization of the structure of the meibomian glands. The clarity the LipiView provides was recently enhanced with the addition of Dynamic Meibomian Imaging (Figure 1). Used in conjunction with the LipiView, the Korb Meibomian Gland Evaluator (TearScience) enables standardized, repeatable evaluation of meibomian gland function at the slit lamp.
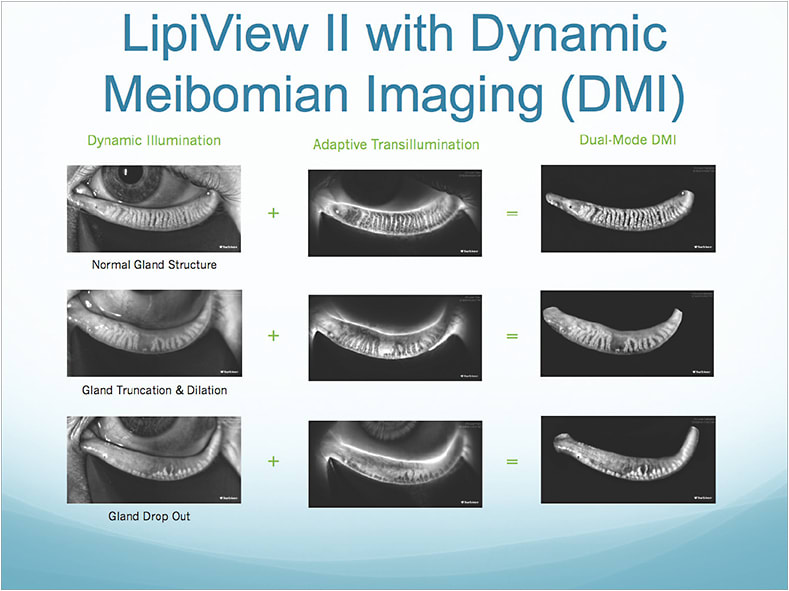
Figure 1. Dynamic Meibomian Imaging from TearScience is based on two novel imaging technologies: dynamic illumination and adaptive transillumination.
All of the tests related to dry eye and meibomian gland disease (MGD) are revenue-generators for a practice, some more so than others. They fuel the dry eye segment of your practice by allowing you to uncover more ocular surface disease, schedule more patient visits, and provide more treatments.
Re-Appointment and Treatment
Scheduling dry eye treatments separate from routine exams and dry eye testing — for example, re-appointing patients for subsequent visits — is key to ensuring you’re being paid appropriately for your services. Re-appointments are a staple in most medical care models, in which patients are rarely, if ever, diagnosed and treated on the same day. The subsequent appointments for patients you’re diagnosing and treating for dry eye can be level II, III or IV encounters, depending on the extent of the history, exam, and medical decision-making.
The dry eye treatment armamentarium has been expanding. In addition to treatments that have been used for years, such as manual meibomian gland expression and punctal occlusion, we can also make use of newer in-office options that take into account the connections between dry eye and lid disease, MGD, and demodex. These include the microblepharoexfoliation BlephEx treatment (Rysurg), the LipiFlow thermal pulsation treatment (TearScience), and the Cliradex Complete eyelid- and eyelash-cleansing treatment (Bio-Tissue). For patients with advanced, chronic, or recurring ocular surface disease, the Prokera biologic corneal bandage (Bio-Tissue), a self-retained, cryopreserved amniotic tissue, can be used to reduce inflammation and promote healing.
In our practice, we also sell a variety of ancillary products to help patients manage their signs and symptoms, such as eyelid cleansing pads, Cliradex moist towelettes warm and cool compress gear, moisture chambers, artificial tears, and HydroEye nutritional supplements (ScienceBased Health). Although our original intent was to bolster patient compliance by making carefully chosen products easily available, we learned that the merchandising adds significantly to our profit margin for dry eye-related care.
Real-world Numbers
I find that most of my dry eye patient visits qualify as level III encounters for insurance purposes. In my state of Nevada, the payment for a level III visit ranges from $74.09-$88.63. And, depending on where a patient is in his treatment plan and what we’re doing at a given visit, I may be billing the third-party carrier or the patient for any of the following in addition to the visit itself (ranges encompass Medicare and private insurers):
• Punctal occlusion OU ($231.24-$264.21)
• Anterior segment photos ($17.35-$57.78)
• Prokera ($1,489.02-$2,532.51)
• Osmolarity testing ($12.57-$23.47)
• InflammaDry ($10.57-$19.42)
• LipiView ($65-$150)
• LipiFlow OU ($950-$2,000) NOTE: TearScience recently reduced the price of its single-use activators, and I recently lowered my charge to patients given that I perform a high volume of treatments.)
• Manual meibomian gland expression ($125-$300)
• BlephEx ($150-$250)
• Cliradex Complete Demodex treatment ($125-$200)
• Nutritional supplements ($395.40, or $161 net for a year’s supply)
• Lid scrubs, artificial tears, eye masks, and so on. ($196 per patient net in a year)
These are a few actual examples from my practice, which illustrate the services a patient received and the revenue they generated:
■ 4 visits, artificial tears, eyelid scrubs, diagnostics (net $577)
■ 4 visits, punctal plugs, artificial tears, eyelid scrubs, diagnostics (net $768)
■ 4 visits, punctal plugs, artificial tears, eyelid scrubs, diagnostics, BlephEx (net $948)
■ 6 visits, punctal plugs, artificial tears, eyelid scrubs, diagnostics, BlephEx, LipiView, LipiFlow (net $1,556)
■ 6 visits, punctal plugs, artificial tears, eyelid scrubs, diagnostics, BlephEx, LipiView, LipiFlow, 1 Prokera (net $2,464)
■ 6 visits, punctal plugs, artificial tears, eyelid scrubs, diagnostics, BlephEx, LipiView, LipiFlow, 2 Prokera (net $3,272)
Creating Value
As you can see, the value we can provide to our patients by utilizing the latest dry eye tests and treatments to diagnose and manage them is matched by its significant contribution to the practice bottom line. •

| Dr. Devries is a co-founder of Eye Care Associates of Nevada, a statewide medical/surgical practice, where he is the clinical director and director of the Optometric Residency Program. |



