KEEP YOUR EYE OUT FOR THIS COMMON ANTERIOR SEGMENT CONDITION
EPITHELIAL BASEMENT membrane dystrophy (EBMD) can be a pain (pun intended) for both the doctor and patient. Doctors can easily miss the subtle anterior corneal findings, and patients can present with vague complaints with this condition. As doctors, we need to look a little closer to make sure we don’t miss the diagnosis and fail to help improve these patients’ symptoms.
Here, I provide an overview of EBMD, its diagnosis and the current treatment options for associated recurrent corneal erosions (RCE) — most of which are well within our scope of practice.
| EBMD (right eye) | H16.321 |
| EBMD (left eye) | H18.322 |
OVERVIEW
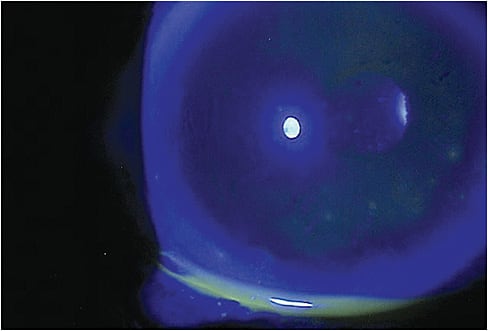
EBMD is also known as map-dot fingerprint dystrophy, in reference to the map, dot and fingerprint-like changes seen in the anterior cornea via slit lamp exam. These areas correspond to thickened, multilaminar or reduplicated basement membrane that can protrude into the epithelium.1
EBMD is predominantly regarded as a degenerative condition, however, a recent study suggests a subset of patients may have genetic mutations associated with EBMD.2 The symptoms and signs of EBMD typically arise in patients in their 40s and 50s and don’t trend toward a progressive decline, but seem to fluctuate through time.1 EBMD is typically bilateral but can present asymmetrically, and is slightly more common in women.
EBMD is also commonly associated with RCEs, which tend to be smaller, yet more frequent than RCEs due to prior corneal trauma.3 RCEs secondary to EBMD are thought to be caused by faulty adhesion of the epithelium to its basement membrane and Bowman’s layer.4 While the EBMD patient sleeps, the closed lid environment creates subsequent corneal edema, which is thought to further weaken epithelial adhesion. Upon waking, the shearing force of the lid against the corneal epithelium can result in a painful erosion.
Interestingly, patients with RCE secondary to EBMD have been found to have over-active matrix metalloproteinases (MMP-2 and -9), which are thought to further disrupt the adhesion of their epithelium to their underlying basement membrane. Also, these patients have been found to be more frequently plagued by MGD and ocular rosacea, which are associated with increased free fatty acids and MMP-9 on the ocular surface.5
DIAGNOSIS
To avoid missing the subtle anterior corneal changes associated with mild EBMD, look for areas of negative staining using a fluorescein strip in lieu of fluorescein sodium/benoxinate solution, as the thicker combination solution may mask these findings. Utilizing retro-illumination during a dilated exam also may bring subtle corneal changes to light. Further, manual keratometry or topography allows for the opportunity to observe an irregular corneal surface due to EBMD. The chosen method of identification is up to you, the doctor.
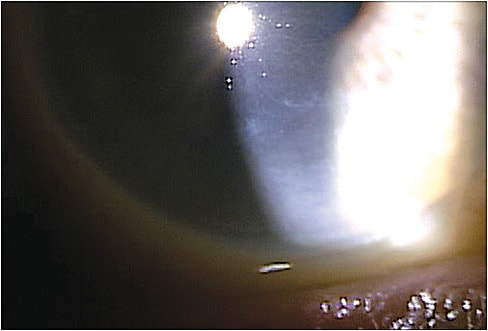
Clinical signs of RCE secondary to EBMD can present as small areas of punctate stain or a more obvious area of absent epithelium via slit lamp. In the case of smaller erosions, the epithelium may be healed by the time the patient is examined, requiring you to dig deeper into the patient’s chief complaint and history to nail the diagnosis. When digging deeper, ask the patient to give a detailed account of the timing and onset of symptoms to elicit responses of pain, foreign body sensation, light sensitivity and tearing upon waking. Also, ask the patient whether he or she recalls any prior incidents with similar symptoms.
TREATMENT
In cases of EBMD contributing to unreliable or difficult refractions, it often helps to treat any concomitant dry eye prior to prescribing glasses or contact lenses, as dryness can exacerbate the fluctuating vision associated with EBMD.
For a short-term fix, consider prescribing preservative-free artificial tears, used every one to two hours, and have the patient return in one to two weeks for refraction. Many patients may benefit from long-term dry eye therapies, including (cyclosporine ophthalmic solution 0.05%, [Restasis, Allergan]/lifitegrast ophthalmic solution 5%, [Xiidra, Shire]) b.i.d., autologous serum tears, an omega fatty acid oral supplement and punctal plugs, just to name a few of the options in the dry eye arsenal.
Keep in mind, EBMD patients with persistent visual symptoms may best be served by you fitting a scleral or traditional RGP lens. These lenses will help mask irregular astigmatism and resolve monocular double vision or shadowing that does not resolve with glasses or soft contact lenses.
For patients who have RCE secondary to EBMD, treatment should be aimed at re-epithelialization of the defect, pain management and the prevention of future erosions. When dealing with a small erosion, prescribing preservative-free artificial tears every hour can help facilitate re-epithelialization. Topical NSAIDs can aid in pain reduction, but should be used sparingly to minimize the delayed healing associated with these medications.
For larger erosions, consider bandage contact lenses that have a flat base curve (to allow lens movement/prevent tight lens syndrome) to aid in pain management until the defect heals. Some advocate leaving the lens on for up to six weeks to promote basement membrane remodeling. Concurrent topical antibiotics for prophylaxis should accompany bandage contact lens wear until re-epithelialization is accomplished.
With regard to the prevention of future erosions, consider treating any evident MGD or rosacea blepharitis with oral doxycycline 20mg to 50mg b.i.d. PO for one to three months.5,6 Along with topical corticosteroids, q.i.d. Doxycycline works to inhibit MMPs associated with weakened adherence of the epithelium to the basement membrane.5,6 Erythromycin ointment nightly or azithromycin 1% solution b.i.d. can also be prescribed to reduce MMP activity, which can be an alternative for the patient who is intolerant to oral doxycycline or as adjunctive therapy.7 Hypertonic sodium chloride ophthalmic drops or ointment, 5% can be used q.i.d and q.p.m., respectively, to improve adherence of the epithelium by reducing corneal edema.
When RCE is recalcitrant, consider performing one of the following procedures to reduce the rate of recurrence and improve symptoms related to EBMD.
- Anterior stromal puncture. This can be performed under topical anesthesia at the slit lamp. Using a 25-gauge bent needle (bent to prevent perforation), shallow punctures spaced 0.5mm apart through the area of erosion as well as the surrounding area of cornea creates the formation of microscopic scars that aid in epithelial adhesion.8 Post-operative pain can be managed with topical NSAIDs, and topical antibiotics are used for prophylaxis.
- Debridement of loose epithelium under topical anesthesia with a surgical spear or blunt spatula.9-11 It is best to avoid sharper instruments to prevent damaging Bowman’s membrane and penetrating the anterior stroma, which can cause significant corneal haze. If you are not sure whether the epithelium is tightly adhered prior to debridement, apply a dry, spear-shaped cellulose sponge to an area of epithelium, and twist. Loose epithelium will be mobile, while normally adherent epithelium will not. Debridement at the limbus should be avoided when possible to preserve limbal stem cells, which are necessary for re-epithelialization and maintenance of corneal integrity.
- Diamond burr polish. After simple debridement, a diamond burr polish of Bowman’s layer to remove residual abnormal basement membrane may allow for a smoother surface for corneal epithelial adhesion. Diamond burr polish after epithelial debridement has been associated with lower rates of recurrence than debridement alone.10
Following debridement and diamond burr polish, a bandage contact lens should be placed to reduce pain and allow re-epithelialization. Prescribing prophylactic topical antibiotics while a bandage contact lens is in place is advised. - Amniotic membrane placement. More recently, authors have advocated for amniotic membrane placement after debridement and polish. Amniotic membranes are utilized for their wound healing, anti-inflammatory and MMP-inhibiting action on the cornea.
Referral for phototherapeutic keratectomy (PTK) is a final option for patients with symptomatic EBMD with or without recurrent RCE.12 Since LASIK is contraindicated in patients with EBMD, due to the risk of epithelial sloughing, PRK at the time of PTK is an alternative that would allow refractive error correction along with EBMD treatment. However, small comparative studies show that debridement with diamond burr polish has a lower rate of recurrence of RCE when compared to PTK.13,14 Since debridement and polish is also simpler and less costly than PTK, it is considered the preferred procedure of the two when performed due to RCE. Thus, PTK is likely best kept for patients interested in refractive surgery or those who have failed treatments with debridement and polish and are looking for other options. OM
REFERENCES
- Rathod D, Nicholson A, Bid B. Corneal epithelial basement membrane dystrophy. Bombay Hosp J. 2009; 51: 126-128.
- Evans CJ, Davidson AE, Carnt N, et al. Genotype-phenotype correlation for TGFBI corneal dystrophies identifies p. (9G623D) as a novel cause of epithelial basement membrane dystrophy. Inves Ophthalmol Vis Sci. 2016; 13:5407-5414.
- Heyworth P, Morlet N, Rayner S, et al. Natural history of recurrent erosion syndrome—a 4 year review of 117 patients. Br J Ophthalmol. 1998; 82: 26-28.
- Xu K, Kam K, Young A, Jhanji V. Recurrent corneal erosion syndrome. Asia-Pac J Ophthalmol. 2012;1: 349-354.
- Dursun D, Kim MC, SOlomon A, Pflugfelder SC. Treatment of recalcitrant recurrent corneal erosions with inhibitors of matrix metalloproteinase-9, doxycycline and corticosteroids. Am J Ophthalmol. 2001; 1: 8-13.
- Wang L, Tsang H, Coroneo M. Treatment of recurrent corneal erosion syndrome using the combination of oral doxycycline and topical corticosteroid. Clin. Exp Ophthalmal. 2008; 1: 8-12.
- Bremond-Gignac D, Chiambaretta F, Milazzo S. A European Perspective on Topical Ophthalmic Antibiotics: Current and Evolving Options. Ophthalmol Eye Dis. 2011; 3: 29-43.
- Avni Zauberman N, Artornsombudh P, Elbaz U Goldich Y, Rootman DS, Chan CC. Anterior stromal puncture for the treatment of recurrent corneal erosion syndrome: patient clinical features and outcomes. Am J Ophthalmol. 2014; 2: 273-279
- Aldave AJ, Kamal KM, Vo RC, Yu F. Epithelial debridement and Bowman’s layer polishing for visually significant epithelial irregularity and recurrent corneal erosions. Cornea. 2009; 10:1085-1090.
- Soong H, Farjo Q, Meyer R, Sugar A. Diamond burr superficial keratectomy for recurrent corneal erosions. Br J Ophthalmol. 2002; 3: 296–298.
- Vo RC, Chen JL, Sanchez PJ, Yu F, Aldave AJ. Long-term outcomes of epithelial debridement and diamond burr polishing for corneal epithelial irregularity and recurrent corneal erosion. Cornea. 2015; 10: 1259-1265.
- Germundsson J, Fagerholm P, Lagali N. Clinical outcome and recurrence of epithelial basement membrane dystrophy after phototherapeutic keratectomy a cross-sectional study. Ophthalmology. 2011; 3: 515-522.
- Sridhar MS, Rapuano CJ, Cosar CB, Cohen EJ, Laibson PR. Phototherapeutic keratectomy versus diamond burr polishing of Bowman’s membrane in the treatment of recurrent corneal erosions associated with anterior basement membrane dystrophy. Ophthalmology. April 2002; 4: 674-679.
- Suri K, Kosker M, Duman F, et all Demographic patterns and treatment outcomes of patients with recurrent corneal erosions related to trauma and epithelial and Bowman layer disorders. Am J Ophthalmol. 2013; 6: 1082-1087.




