One of the most significant discoveries related to the diagnosis and management of dry eye has been that evaporative dry eye caused by meibomian gland dysfunction (MGD) is likely far more prevalent than dry eye caused by tear deficiency. In one study, Lemp and colleagues found that among patients diagnosed with dry eye in 10 clinics in the European Union and the United States, 86% demonstrated signs of MGD.1 Like dry eye disease, MGD is a complex entity, and the two are intertwined in the same cycle that, without appropriate treatment, can lead to ocular surface damage.
THE PATHOPHYSIOLOGY OF MGD
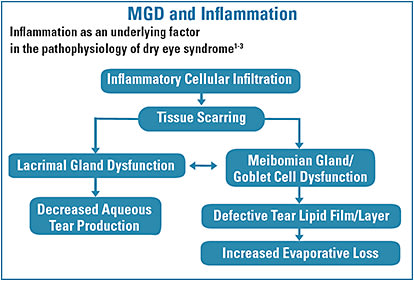
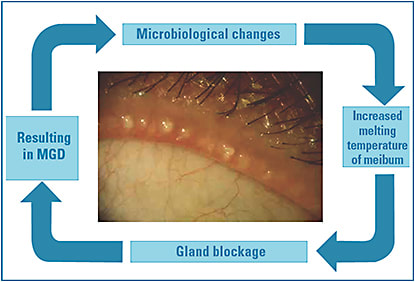
One of the pathophysiological mechanisms common to both dry eye and MGD is inflammation. Inflammation leads to tissue scarring, which causes lacrimal gland dysfunction and decreased aqueous tear production. But inflammation and tissue scarring also lead to MGD and goblet cell dysfunction, both of which can create a defective tear film lipid layer, in turn causing increased evaporative tear loss (Figure 1). Five physiological mechanisms of MGD are known: eyelid inflammation, conjunctival inflammation, corneal damage, microbacterial changes, and dry eye from tear instability.2 Clearly, MGD is multifactorial, and these factors tend to be cumulative. For example, MGD can begin with microbial changes at the lid margin, which initiates a self-stimulating cycle (Figure 2). Bacterial changes lead to hyperkeratinization and an increase in the melting temperature of the meibum, which leads to gland blockage and eventual meibomian gland dysfunction. With the glands compromised, tear instability, hyperosmolar tears, and inflammation ensue.
TREATING MEIBOMIAN GLAND DISEASE
LipiFlow (TearScience) is the first device approved by the FDA for the treatment of MGD. I’ve used this 12-minute procedure as part of treatment for about 100 patients and have achieved good results. Many patients have described the treatment as “spa-like.” One study that pertains to patient selection for LipiFlow is worth mentioning. The purpose of the study was to determine if meibography can predict meibomian gland function in patients with symptoms of dry eye (based on the SPEED questionnaire).3 The researchers performed meibography using the Modi topographer and Phoenix software (s4optik) and measured gland function and estimated functional gland volume using the Korb Meibomian Gland Evaluator (TearScience). They found that the nasal and central sections of the lower eyelid contained the highest average number of glands and significantly more functional glands and higher functional gland volume than the temporal section. However, somewhat counter-intuitively, the amount of gland atrophy was significantly highest in the nasal section, and the atrophy didn’t correlate with gland function or volume (except in the case of total gland dropout). While this was a small study involving 23 eyes, the take-home message for me is that if meibography shows gland atrophy, it doesn’t necessarily mean LipiFlow treatment won’t be successful. We still may be able to stimulate the glands to fully function and relieve symptoms.
I also use intense pulsed light therapy (IPL, DermaMed) for patients with MGD. IPL was originally developed to address irregular skin pigmentation but has been reengineered for this new use. A treatment involves six to eight pulses of Xenon flash lamp light applied to the malar region on each side of the face. The mechanism of action isn’t fully understood. It may be related to a decrease in bacterial load, or the regression of telangiectasia, but it has worked very well for select patients in my practice. That said, we must be aware that IPL shouldn’t be performed on patients who have darker skin; it’s safest for those with skin types 1 to 5 on the Fitzpatrick scale.
BlephEx (Rysurg), which we usually think of as a treatment for Demodex and blepharitis, can be effective for MGD, too. BlephEx is essentially exfoliation for the lid margin. Using the handpiece and micro-sponge along the edge of the eyelids and lashes, the clinician removes excess debris, bacteria, and biofilm that can lead to inflammation and dry eye problems. In a study of 20 patients with MGD who were examined and tested prior to and 4 weeks after one BlephEx treatment, mean score on the Dry Eye Ocular Surface Disease Index questionnaire improved by 53%, mean tear break-up time improved by 65%, and mean severity of both blepharitis and MGD on the Efron scale improved by 54%.4
Although most of our treatments for MGD are on the outside of the body, we can also work from the inside by recommending omega fatty acid supplements. TheraTears Eye Nutrition (Akorn) and HydroEye Support for Dry Eyes (ScienceBased Health) are two options. The TheraTears product provides omega-3s (EPA, DHA, ALA) from fish oil and flaxseed. HydroEye contains the omega fatty acid GLA, which is derived from black currant seed oil, as well as omega-3s (EPA, DHA) from fish oil. Most of my patients who are using HydroEye are dedicated to taking it. Several patients say they can tell when they miss a dose.
MGD CLINICAL TIP
Staining the Line of Marx with vital dye, lissamine green in particular, can serve as a fast and simple indicator of meibomian gland dysfunction (MGD).1 Marx’s Line is a row of cells located on the upper and lower eyelid at the junction of keratinized eyelid epithelium and palpebral conjunctiva. As evaporative dry eye progresses, the line shifts. It moves from behind the meibomian glands (entirely on the conjunctival side) to partly touching the glands, to transecting the glands, to in front of them (entirely on the eyelid margin side).
As you can imagine, when this thickened line of cells interferes with blinking, meibum isn’t able to reach the ocular surface properly.
Reference
- Yamaguchi M, Kutsuna M, Uno T, Zheng X, Kodama T, Ohashi Y. Marx line: fluorescein staining line on the inner lid as indicator of meibomian gland function. Am J Ophthalmol. 2006;141(4):669-675.
MORE TO LEARN
Our current treatments for MGD are a big help for patients and for us as we manage this potentially complicated and uncomfortable condition. Our understanding of the disease will continue to improve and bring us additional therapies to help patients that much more.

REFERENCES
- Lemp MA, Crews LA, Bron AJ, Foulks GN, Sullivan BD. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: a retrospective study. Cornea. 2012;31(5):472-478.
- Baudouin C, Messmer EM, Aragona P, et al. Revisiting the vicious circle of dry eye disease: a focus on the pathophysiology of meibomian gland dysfunction. Br J Ophthalmol. 2016;100(3):300-306.
- Murakami D, Blackie CA, Pult H, Korb DR. Meibomian gland function cannot be predicted by meibography in patients symptomatic for dry eye. Invest Ophthalmol Vis Sci. 2014;55(13):27.
- Connor CG, Choat C, Narayanan S, Kyser K, Rosenberg B, Mulder D. Clinical effectiveness of lid debridement with BlephEx treatment. Invest Ophthalmol Vis Sci. 2015;56(7):4440.




