Tracing the tracks of her tears
Both punctum (those that rest on top of the puncta) and intracanalicular (those that are either within the horizontal or vertical nasolacrimal canaliculus) punctal plugs are commonly recommended management options for patients who have dry eye disease (DED). Additional indications for this important treatment modality are ocular dryness related to refractive or corneal surgery and conditions, such as recurrent corneal erosion and superior limbic conjunctivitis.
Specifically, punctal plugs can provide relief to patients who have the aforementioned conditions by preventing the tears from draining. In recognizing the enormous relief these tiny devices can provide to such patients, I am an active prescriber. That said, punctal plugs, as is the case with all treatments, are not without possible adverse events.
Here, I discuss one such event, and pearls for its prevention.
| Keratitis | H16 |
| Epiphora | H042 |
| Stenosis and insufficiency of lacrimal passages | H04.5 |
THE EVENT
A 43-year-old, healthy female patient who had severe DED experienced repeated extrusion, or spontaneous loss of her punctal plugs altogether, despite changes in plug size and shape. (Extrusion is thought to be related, in part, to the shape of the plug relative to the patient’s eyelid and nasolacrimal anatomy. It is typically reported within the first few months of insertion, however, it has been seen up to two years later.)
The repeated extrusion ultimately led to the insertion of a completely different punctal plug design. Nevertheless, three months later the patient returned with the complaint, “it’s working too well in my right eye.”
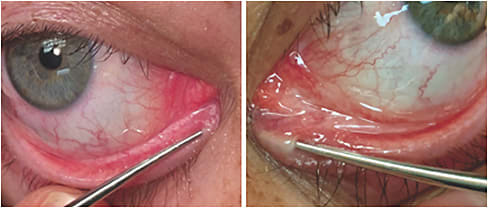
Examination revealed epiphora secondary to a physically stenosed nasolacrimal system, or obstruction of the nasolacrimal duct. While uncommon, this has been reported and should, therefore, be considered in any case of excessive tearing following punctual plug placement. While stenosis is rarely reported in the literature, some studies show an incidence of up to 18%, reports the American Journal of Ophthalmology. Since patients undergoing punctal occlusion are doing so because they need retention of tears, most with stenosis do not complain, so it may often go undiagnosed. Jones No. 1 and Jones No. 2 tests and, in some cases, simple punctal dilation can confirm the diagnosis. (See photos.)
Stenosis is most often associated with spontaneous extrusion, occurring within three months after loss of the plug. The cause is unknown, but according to the Journal of Ophthalmology, it is thought to be related to scarring of the punctal mucosa or inner canalicular wall from the initial procedure (e.g. dilation, insertion of plug itself) and/or slanted contour of some plugs. In the case of this patient, anatomical angle as well as small diameter of her puncta necessitated fairly aggressive dilation prior to insertion, supporting these speculations.
Once determined that the patient had stenosis of the nasolacrimal system, a topical steroid paired with warm compresses and digital massage of the area adjacent to the blockage was prescribed. In her case, symptoms subsided and no further treatment was pursued. However, perforated punctum plugs offer a possible solution, as they allow tears to flow through an otherwise collapsed or dysfunctional drainage system. Surgical options, such as dacryoplasty, may also be considered in cases with recalcitrant stenosis and progressed symptoms.
PEARLS FOR PREVENTION
In addition to the extrusion, epiphora and punctal stenosis seen in this patient, punctal plugs can also result in migration, granulation of tissue within the nasolacrimal system, puncta enlargement, pyogenic granuloma, canaliculitis, dacryocystitis and biofilm build up. To reduce the likelihood of these complications, O.D.s should:
- Evaluate the punctal plug post-insertion for proper fit relative to the lid nasolacrimal anatomy size and shape. The plug should be snug and flush with the punctum and rotated, if necessary.
- Prescribe a mild steroid or combination antibiotic at insertion time to quell any possible inflammatory reaction that may lead to granulation or scarring, and to prevent infection and biofilm.
- Educate the patient regarding proper lid hygiene. We should consider prescribing a lid wipe or foam to supplement the plugs, particularly to help prevent biofilm and debris build up.
- Educate the patient that if the punctal plug seems to have been lost or has fallen out, she should return for care as soon as possible. We should consider a steroid at this point to prevent stenosis.
- Consider extended-duration dissolvable plugs in cases of frequent extrusion. OM




