A look at what to be aware of and how to manage these patients
Minimally invasive glaucoma surgery, also known as MIGS, is a well utilized option for ophthalmologists to surgically manage glaucoma patients. The reasons: A MIGS procedure can help to reduce the patient’s glaucoma dosing regimen, while preventing unnecessary disease progression. As is the case with traditional glaucoma surgeries, O.D.s can play a co-management role to boost the probability of an excellent outcome.
Here, I discuss the specific co-management considerations associated with MIGS.
IOP SPIKES
Typically, IOP spikes can occur post-op day one and out until one-month post-op. The majority of IOP spikes can be controlled with one or two topical glaucoma drugs, as many of these patients have mild to moderate glaucoma.
If the IOP spike is severe (around 40 mmHg), the addition of an oral anti-glaucoma drug to topical glaucoma drugs may be needed. Specifically, the tapering of postoperative steroid use, along with use of topical glaucoma drugs, can reduce IOP.
HYPHEMA
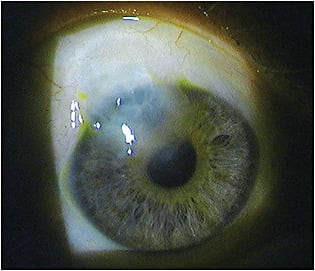
A mild, transient hyphema is not uncommon with MIGS and appears on slit-lamp exam similar to an anterior chamber reaction you might see after cataract surgery or with a mild iritis.
Hyphema is not urgent, so the patient can continue his normal postoperative regimen and be monitored until hyphema resolution occurs, around one-week post-surgery. It is important pre-operatively to tell the patient of the possibility of a small hyphema, so he does not panic upon slightly blurry vision.
HYPOTONY
Patients who undergo subconjunctival MIGS can experience hypotony, as episcleral venous pressure is being bypassed.
The literature varies a bit, but typically hypotony manifests as less than between 6.5 mmHg and 5 mmHg. If the anterior chamber is formed, and on retinal exam no choroidal effusions or folds are noticed, monitoring the patient is the management approach. Additionally, the patient’s topical glaucoma drugs should be stopped, so that IOP can rise. If, however, the anterior chamber is flat or significant choroidal effusions or folds exist, a referral back to the surgeon is warranted for an anterior chamber fill with a viscoelastic.
Bleb-related complications also need to be considered for these patients — low-lying filtering bleb — and include erosion of the MIGS device through the conjunctiva, leading to a leaking bleb or blebitis, fibrosis and encapsulated bleb. A leaking bleb will render a positive Seidel test, and a clear, almost white bleb with anterior chamber reaction is noted with blebitis.
In summary, the following tests should be performed on every MIGS patient: slit lamp, gonioscopy — at least once in the postoperative period if the patient has undergone a MIGS — NaFl staining to look for Seidel, otherwise not necessary, IOP and an anterior chamber evaluation to look for cell and flare.
CO-MANAGEMENT IMPORTANCE
The Association of American Medical Colleges estimates a shortage of surgeons, including ophthalmologists, by 2025. This means they’ll depend on O.D.s for their co-management prowess. Get up to speed on co-managing MIGS, and inform local M.D.s about your skills. (See this article online for MIGS Co-Management Coding.) OM




