More than 60% of respondents to the 2018 GP Annual Report indicated that scleral lenses have increased slightly, and almost 20% of respondents reported that scleral lens fitting has increased greatly.1 This growth makes sense, when one considers the myriad indications for scleral lenses: ocular surface rehabilitation in severe ocular surface disease, vision improvement by correcting corneal irregularities from corneal ectasias, recovery following corneal surgery and, most recently, refractive error correction, including presbyopia in normal, healthy eyes. To serve these patients, practitioner’s expertise is coupled with instrumentation and proper fitting to result in excellent patient outcomes. With this in mind, here’s a look at the instruments one can use to aid in ensuring proper scleral lens fitting, based on prescribing needs and practice goals.
COVERING THE BASICS
For beginners, the absolute minimum technology needed to apply a scleral lens on an eye and evaluate the findings is a slit lamp. The slit lamp allows the practitioner to evaluate the landing zone; additionally, a white light slit beam is used with sodium fluorescein to evaluate the clearance. An ideally fit scleral lens will clear the entire cornea and limbus, without limbal bearing, to land on the scleral conjunctiva. To achieve this, the practitioner must evaluate corneal diameter to select the appropriate scleral lens diameter, the initial diagnostic lens set and sagittal depth. Thus, large corneas will likely need a somewhat larger overall diameter lens, and smaller corneas may require a smaller diameter lens. If the scleral lens touches the cornea, the sagittal depth should be increased. If the scleral lens has excessive clearance, the sagittal depth should be reduced. It is vital to clear the limbus, as it gives rise to new corneal epithelial cells.2
IMAGING THE CORNEA
The following imaging platforms are valuable to provide documentation of baseline findings prior to scleral lens fittings and, along with careful note-taking, help practitioners to optimize management strategies during the fitting process by defining areas of elevation or depression on the ocular surface. Listed in the order a practitioner may follow to build on their practice, a corneal topographer is suitable for most who fit scleral lenses. Corneal tonometry and anterior segment OCT can be added to a practice’s tools, as practitioners increase their familiarity with more fitting sets.
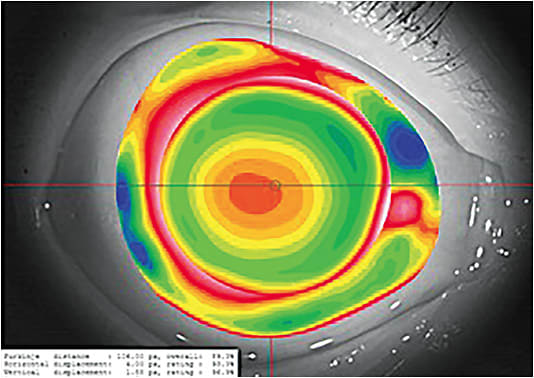
Corneal topography. Most corneal topographers are Placido disc reflection systems and project a series of concentric rings or colored dots on the cornea; the distances between the reflections are then measured and analyzed.3 There are practical limitations in the peripheral cornea where the values either become less reliable, and/or the instrument is unable to measure the entire area.4,5 A corneal topographer should image the entire cornea. The average corneal diameter is 11.71 mm.
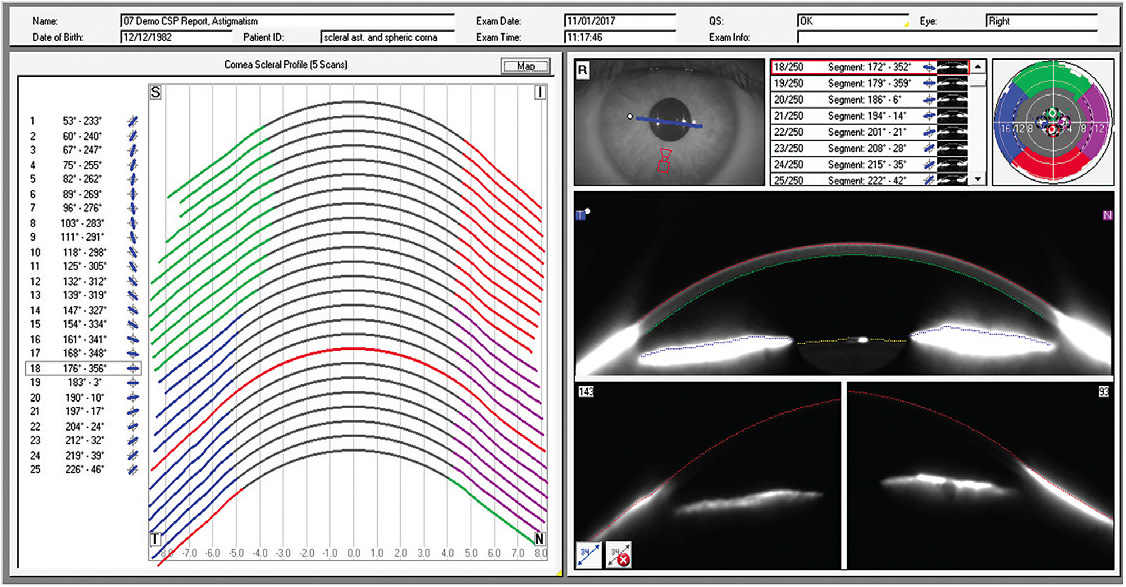
Corneal tomography. Scheimpflug imaging is one of the techniques used in corneal tomographers to scan optical sections of the cornea, thus creating a full elevation map of both the anterior and the posterior cornea. (Optical slit-scan is the other technique.) Scheimpflug systems typically cover a large corneal area, but are limited to the corneal surface. A newly developed software update is able to provide a corneo-scleral section in addition to corneal data.5 The software provides information about corneal curvature, such as elevation and depression information, as well as scleral topography information.
Anterior segment OCT. This instrument offers a cross-sectional image of a scleral lens on an eye. The clearance between the posterior lens surface and the cornea can be determined using the instrument’s caliper tool to measure vault. This measurement provides an accurate evaluation of the lens clearance. Anterior segment OCT also can confirm whether the scleral lens is clearing the conjunctival elevation and may be used to evaluate the edge alignment of scleral lenses on the conjunctiva and underlying sclera. This is particularly helpful when there are conjunctival elevations, such as pingueculae, pterygium, glaucoma blebs or scleral patch grafts. However, there are limitations on how far an OCT can measure in primary gaze. Since scleral lenses are in large diameters, a scan may not be able to capture the entire scleral lens.
EVALUATING SCLERAL SHAPE
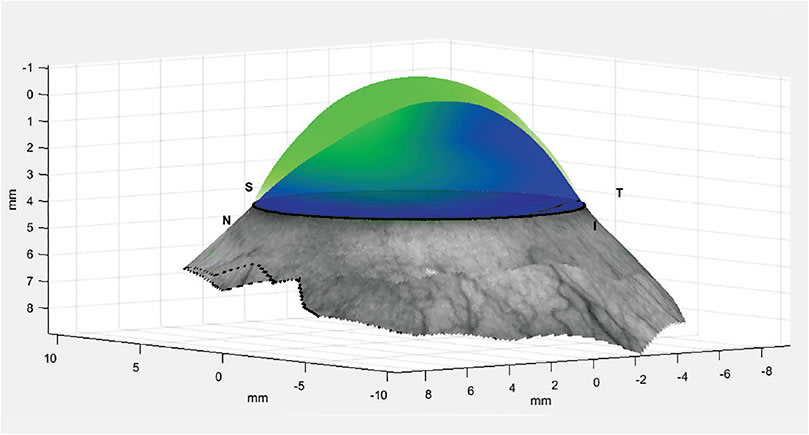
Scleral topographers, or profilers, are instruments that display the depth and shape of the cornea, as well as the shape of the sclera. These instruments are valuable in determining whether toricity is needed in the scleral landing zone. Three instruments are available. Each output values, such as lens diameter, sagittal heights (cornea and scleral) and toricity value, allow you to match the patient with the appropriate scleral lens or provide design information for a custom lens.
Scleral topography is helpful for anyone fitting scleral lenses. For those fitting a lot of scleral lenses, scleral topography information is advantageous. Even if the cornea is not highly irregular, the sclera may be, complicating a fit. Thus, this technology can be helpful for everyone.
PRESCRIBING CUSTOM SCLERAL LENSES
Scleral lens specialists, specifically, will benefit from impression-based scleral lens technology. For difficult situations, scleral lenses can be custom made from an impression, or mold, of the eye. Impressions are helpful for extreme corneal irregularity, significant ocular surface asymmetry or localized corneal or conjunctival irregularities in which the peripheral curves or diameter of a scleral lens cannot be modified. Even with lens modifications of a diagnostic lens, compression, or edge lift, may be present in one or more areas of the lens. Ocular surface irregularities include pingueculae, pterygium, blebs and glaucoma drainage devices. Patients who have moderate elevation of the ocular surface and highly irregular corneas, such as a proud plateau graft or advanced nipple cone, can benefit from this technology, of which there is one available on the market in the U.S.
CORRECTING ABERRATIONS
As the ability to measure and quantify scleral contour and higher-order optical aberrations expands, scleral lenses may become an ideal delivery platform for accurate and stable correction of higher-order aberrations; thus, practitioners hoping to treat these patients may find aberrometers useful. In eyes that have corneal irregularities, both corneal and scleral rigid GP lenses can neutralize irregularities of the front surface of the cornea. However, aberrations from disparities in the corneal stroma or posterior corneal surfaces are often not addressed in lenses that have standard optics. As scleral lenses are rotationally and translationally stable, they are an ideal platform for the correction of higher-order aberrations.
Lower-order aberrations include defocus and astigmatism, or sphero-cylindrical refractive errors, that can be corrected by conventional spectacles, contact lenses or refractive surgery. Higher-order aberrations including trefoil, coma and quadrafoil refer to irregular astigmatism that cannot be remedied with conventional optical correction.
EQUIP YOUR OFFICE
Whether practitioners are prescribing scleral lenses rarely to correct corneal irregularities or are specialists in the field, technology plays a crucial role in the fitting process. In addition to this article, a multitude of resources on scleral lens fitting are available, including books, such as “Contemporary Scleral Lenses: Theory and Application” (of which I am an author and co-editor); “Clinical Guide to Scleral Lens Success” (of which I am an author) and “A Guide to Scleral Lens Fitting;” magazines, such as Contact Lens Spectrum (also published by PentaVision), specifically my Scleral Lens Monthly column; and groups, including the Scleral Lens Society (sclerallens.org ) and the Gas Permeable Lens Institute (gpli.info ). OM
Billing and Coding
Scleral lenses can often be billed to vision and medical insurances. Each plan has its own requirements that must be researched and followed. Always check with the plan before proceeding with scleral lens fitting and progress visits.
A prior authorization for insurance should be completed, when necessary, before ordering lenses and rendering services. Information for a prior authorization should include the fitting, material and ICD-10 codes. (Codes can be found via GPLI https://www.gpli.info/pdf/specialty-lens-codes.pdf .) This authorization needs to be obtained before billing for medically necessary contact lens fitting and lenses. The lens-fitting code, lens design (scleral lens code) and associated code (keratoconus, ocular surface disease, etc.) should be submitted.
Contact lens fitting and lens material fees may also be considered medically necessary, depending on the patient’s status and the plan.
Advanced Beneficiary Notice (ABN) of Noncoverage is a standardized notice issued to a patient before providing services. An ABN should be issued when you believe insurance may not pay for the service. In addition, a separate contact lens form describing associated fee ranges for services and materials may be signed by the patient prior to the scleral lens fitting. This provides realistic expectations of fees that the patient may have to pay.
REFERENCES
- Bennett, E. GP Annual Report 2018. Contact Lens Spectrum. 2018; 33:20-27, 50.
- Secker, G.A., Daniels, J.T., Limbal epithelial stem cell of the cornea. In Source Stembook [Internet]. Cambridge (MA): Harvard Stem Cell Institute; 2008-2009 (June 30, 2009).
- Bowden T. Contact Lenses – The Story. Kent Bower House Publications; 2009.
- Reddy T, Szczotka LB, Roberts C. Peripheral corneal contour measured by topography influences soft toric contact lens fitting success. CLAO J. 2000; 26: 180-5.
- Szczotka LB, Roberts C, Herderick EE, Mahmoud A. Quantitative descriptors of corneal topography that influence soft toric contact lens fitting. Cornea. 2002; 21: 249-55.




