Arguably, most authorities would say that advances in glaucoma imaging technology, medications, laser and filtering surgery over the past 40 years are at least parallel to, if not exceeding, most other subspecialties in optometry and ophthalmology. (Of course, this is mentioned with great respect for the profound developments in essentially every topical field of ophthalmic care.)
As a result of these advances, for the past several years, the pendulum has progressively swung toward optometry as both the entrance portal for glaucoma diagnosis and, increasingly, a primary provider of medical management of this disease. Underpinning this shift are many factors, which include affordability of diagnostic equipment for optometric in-office use, extraordinary developments with identifying exquisite optic disc structure and retinal nerve fiber layer (RNFL) thickness, novel software programs that enable progression analysis, and a cafeteria of topical treatment options to manage IOP. As leading advocates for vision loss prevention, it is increasingly crucial for optometrists to take ownership of identifying glaucoma suspects and, as indicated, treatment.
Let’s discuss three primary reasons glaucoma should be on our radar.
1 O.D. ACCESS
In Washington state where I practice (topical glaucoma authority 1989, oral drugs in 2003), O.D. practices are in 92% of all state counties, whereas ophthalmology practices are in 69%. This is representative of the U.S., where O.D.s practice in over 10,000 communities that serve 99% of the U.S. population, reports Census data. Additionally, between 35% to 40% of U.S. counties (or county equivalents), representing about 25 million largely rural-based individuals, do not have access to an ophthalmologist, reports the American Medical Association. Access to care and O.D. availability has been a time-honored and powerful argument for intensifying medical training and the drug privileges of optometric physicians to serve patients in more suburban and rural communities.
2 PRIMARY CARE LEVEL DETECTION
Optometry is the provider of about 70% of all primary eye care examinations, according to the most recent Eye Care Workforce study. Additionally, we have the skill set and diagnostic tools to aid us in identifying glaucoma suspects. It’s worth noting that many of the diagnostic devices already used during the annual comprehensive eye health evaluation can aid us in identifying glaucoma suspects. They include a tonometer, a slit lamp, which may show pigment dispersion, pseudoexfoliation and narrow angle, and ophthalmoscopy, which can reveal disc cupping and neural rim asymmetry, among other findings.
Something else to consider: Glaucoma consultation testing and early management by optometrists and ophthalmologists in nearly all states are essentially indistinguishable: We perform the same tests, essentially read the same literature and follow evidence-based guidelines, as published by leading organizations in the field. (Dr. Joshua Clermont delves into the practice management aspects of glaucoma care in “Master Glaucoma Services,” p.30.)
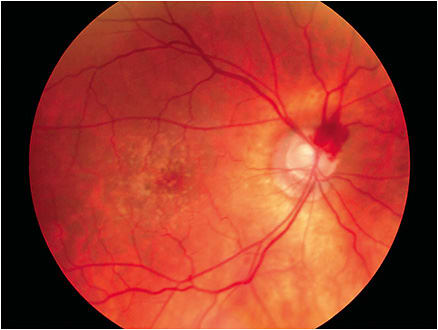
Further, as we gain experience, we become better judges of early changes in glaucomatous disc morphology, expert gonioscopists, proficient VF analyzers of consistent, yet subtle, clustered relative depressions on standard perimetry (24-2 and 10-2) and skillful at interpretations of disc and retinal scanning tomography. Scanning tomography is an excellent resource of both early changes, as well as progression. Many instruments use the patient’s age-related normative database for individual comparison of localized RNFL thickness changes. In summary, as we administer glaucoma care, we establish initial baseline data and then compulsory re-measurements of key indicators of progression: IOP, VF, RNFL and ganglion cell complex (GCC) thicknesses. (See Dr. Andrew Rixon’s article “Catch the Silent Thief,” p.20. for additional information on diagnostic tools that aid in the glaucoma diagnosis.)
3 TRAINING
Medical management of glaucoma is an integral component of optometry school curriculum, many residencies, and it is covered extensively in post-graduate CE. Also, the Optometric Glaucoma Society, Glaucoma Section of the Academy of Optometry and optometry school post-graduate CE programs, among others, provide important resources for staying abreast of research and clinical updates. In all but Massachusetts, O.D.s have the authority to prescribe IOP-lowering drops, if indicated. This includes taking into consideration non-IOP issues, which Dr. John O’Donnell will elaborate on in “Look Beyond IOP in Glaucoma,” p.26.
TAKE ACTION
The pendulum continues to swing toward optometry when it comes to glaucoma care. I hope that this introduction, as well as the diagnostic, therapeutic and practice management articles by Drs. Rixon, O’Donnell and Clermont will encourage O.D.s to augment their glaucoma clinical acumen and play a greater role in the management of this progressive and relentless disease. OM




