Contact lens wear is booming. Thanks to our industry partners, optometrists are seeing an ever-expanding library of soft lens parameters, corneal GP lenses, scleral contact lenses and orthokeratology lenses that we, as eye care providers, can make available to our patients.
Having the right tools in the office can expedite the fitting process of these lenses, while aiding in the monitoring of the progression of ocular diseases, such as keratoconus. With this said, here’s a look at these tools:
TOPOGRAPHY
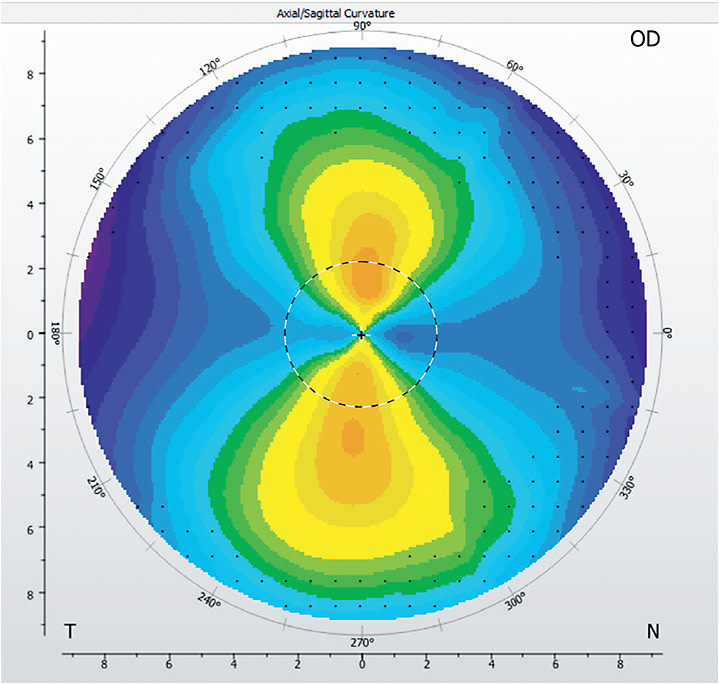
Topographers allow contact lens fitters to quickly estimate how lenses will fit, especially because many modern topographers can extrapolate corneal elevation changes, which can be used to predict where the lenses will settle. This is especially useful for corneal GP contact lens fits on keratoconic eyes, as the elevation topography allows us to visualize the “peak” of the cornea where the lens may settle; in many cases this is significantly inferior to the line of sight.
For patients who have irregular corneas, a topographer’s elevation map can help drive the decision of whether to fit a corneal lens or a scleral lens. This is because research shows that corneas that have less than 350 μm of elevation difference have an 88% chance of success in a corneal GP lens, while corneas that exhibit greater than 350 μm of elevation difference have a higher success rate in scleral lenses.1 Choosing a starting lens modality that may offer a higher level of success before a lens is put on the eye can save chair time, providing a better experience for both the patient and the fitter.
Some of the more advanced topographers also allow the fitter to enter lens parameters and see the fluorescein patterns that would be expected, should that lens be ordered and placed on the patient’s eye.
Beyond these benefits, using a topographer to screen contact lens patients also provides value. In our clinics, we perform topography on every contact lens patient pre-fit or refit. Performing a pre-fit screening topography allows us to quickly screen for corneal irregularities, such as keratoconus, pellucid marginal degeneration, corneal warpage and irregular surface patterns, all of which can affect the contact lens choice. In fact, since we have started performing topography on patients prior to lens fitting, we have come across many patients who show early keratoconic changes, though they have no subjective complaints, and before significant corneal findings were present on biomicroscopy.
In our clinics, we utilize an all-in-one topographer, autorefractor, keratometer to pre-screen patients. If we find that a patient has anterior surface irregularities, such as corneal ectasias, we utilize a stand-alone topographer for an advanced evaluation and monitoring. There is an important distinction in terms of coding for these services. With a large contact lens-wearing population, we find that the additional cost for the screening topographer is well worth the investment, as it brings more patients into contact lens wear and helps us to quickly rule out problems. In regard to return on investment, our rule of thumb is that a new technology should pay for itself within six to 12 months, either through payment or reduction in chair costs.
ANTERIOR SEGMENT CAMERAS
Anterior segment photography can be performed on patients who have corneal pathology, such as corneal scarring, corneal abrasions and dry eye disease, and it is especially useful in the specialty contact lens fitting process. Let us explain.
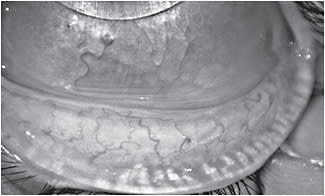
On compromised corneas, such as post-graft corneas, we often take detailed photos of the cornea prior to lens fitting to provide a baseline image, allowing us to easily monitor for changes. During the fitting process, and on regularly scheduled cornea evaluations, we are able to see whether the lenses are causing negative changes, such as impingement, hypoxia or neovascularization. To aid in the fitting process itself with specialty lens fits (corneal GPs, sclerals, orthokeratology and custom soft lenses), photos and videos of the lenses can be sent to the lab consultants for their opinions on lens customization. (Also, this is a fantastic tool to connect with experts in fitting those lenses.)

One such anterior segment camera could be an OCT. Many OCTs have adaptive lenses that allow for anterior segment scans. Similar to topography, anterior segment OCT imaging can be performed to monitor corneal changes during and after specialty lens fits. For example, many OCTs have the ability to perform corneal pachymetry, which can enable fitters to monitor any induced corneal edema during and after a scleral contact lens fit. For specialty scleral lens fits, high-definition images can be taken to measure the precise clearance of the lens over the central cornea, over the limbus and to evaluate edge lift or impingement; these measurements allow for more exact changes to perfect the fit.
Equipment, such as OCTs, among other anterior segment imaging systems, that can be used in many facets of the practice often, are the most beneficial initial investments because they can be used for many different areas, and thus billed for different areas, as you build your contact lens practice. Additionally, multifunctional equipment minimizes the footprint of new equipment, minimizes staff training time and allows for multiple revenue streams that can help to recoup the cost of the machine quickly. (See “Consider Multifunctionality” for more information.)

SPECULAR MICROSCOPES & OPTICAL BIOMETERS
There are many examples of specialized pieces of equipment that contact lens specialists may argue are vital to any contact lens clinic. Two such examples are a specular microscope, which calculates endothelial cellular density, and an optical biometer, which measures axial length.
Specular microscopes serve an important role, especially in scleral lens wearers and post-graft patients, in ensuring the corneal endothelium is healthy enough for scleral wear. In general, a minimum of 400 cells/mm2 to 700 cells/mm2 is thought necessary to maintain corneal health and transparency.2
If myopia management is an integral part of your practice, consider acquiring a device that can monitor and measure axial length progression. Here’s why: A number of studies confirm the correlation between the amount of myopia and axial length.3-6 At our practice, we use a non-contact A-scan.
INTEGRATE TECHNOLOGY INTO THE PRACTICE
Prior to making a purchase, we recommend taking the time to research the differences among similar products, considering the various ways to use the new technology and allowing time for staff to become thoroughly trained in using the equipment. (Previous coverage, “Roll Out New Technology to the Staff” can provide steps at bit.ly/2MQHcBi .) With careful planning, a new piece of equipment can be seamlessly integrated, improve patient care and have a positive impact on the bottom line. OM
Consider Multifunctionality
A KEY FACTOR when choosing a piece of equipment is considering how the new technology can be utilized for more than just contact lens patients. Having such a device can ensure the investment in the device is profitable in the long term.
For example, three topographers on the market have, or will soon have, ocular surface analysis and meibography capabilities. Some even have anterior segment cameras, cobalt blue filters for corneal evaluation and lipid layer analysis. Given that contact lens fits and discovering dry eye disease are so intertwined, utilizing a single piece of equipment for both may be ideal.
REFERENCES
- Zheng et Al. “Corneal Elevation Difference and the Initial Selection of Corneal and Scleral Contact Lenses.” Pacific University College of Optometry. Poster.
- Fadel Dad, Kramer E. di et al. Potential contraindications to scleral lens wear. Contact Lens & Anterior Eye, 2019; 42: 92-103
- Hou W1, Norton TT, Hyman L, Gwiazda J.. Axial elongation in myopic children and its association with myopia progression in the Correction of Myopia Evaluation Trial (COMET). Eye Contact Lens. 2018; 44: 248-259
- COMET Group. Myopia stabilization and associated factors among participants in the Correction of Myopia Evaluation Trial (COMET). Invest Ophthalmol Vis Sci. 2013; 54: 7871-84
- Wong HB, Machin D, Tan SB, Wong TY, Saw SM. Ocular component growth curves among Singaporean children with different refractive error status. Invest Ophthalmol Vis Sci. 2010; 51: 1341-7.
- Hyman L, Gwiazda J, Hussein M, et al. Relationship of age, sex, and ethnic with myopia progression and axial elongation in the correction of myopia evaluation trial. Arch Ophthalmol. 2005; 123: 977-87.





