A 44-year-old male with keratoconus presented to the clinic for the first time with complaints of persistent redness and eye pain from his scleral lens wear OU, though worse pain and photophobia OD. The pain was described as being “pricked by a needle” and was reported as most severe for 5 minutes after lens removal. The patient said he believed both eyes were particularly irritated that day due to allergies, as symptoms seemed more severe after mowing his lawn. He went on to explain that he relies on his scleral lenses to provide functional vision for work and driving, though he immediately removes them when he gets home, due to discomfort.
Upon questioning, the patient said he was compliant with lens cleaning procedures. Additionally, he requested an updated refraction because he said he was desperate for an alternate form of vision correction, even though he reported poor vision with glasses.
On the day of the patient’s initial examination, VA with scleral lenses was 20/20-2 OD and 20/30 OS. Refraction was performed, and BCVA with glasses was, unfortunately, 20/600 OD and 20/450 OS, far below minimum VA requirement for his driver’s license. Scleral lenses would be his best option for maintaining his lifestyle.
Fortunately for this patient, and others like him, the scleral lens industry has made significant advances to increase lens comfort. Here, I discuss these technological advancements by taking you through his individual problems with wear and their solutions.
PROBLEM 1: OCULAR SURFACE DISEASE
An in-depth look at the patient’s medical record revealed well-documented periods of contact lens intolerance with both scleral and soft toric contact lenses.
Diagnostic tools: Ocular history was significant for underlying ocular surface disease, due to blepharitis and chronic allergies, as determined by slit lamp examination with vital dyes, as well as staphylococcus marginal ulcer and bilateral, central corneal abrasions from scleral lens wear.
Solution: As a healthy ocular surface is critical for a successful scleral lens fit, I prescribed a short course of a prophylactic antibiotic drop and the temporary removal of lens wear OD, as this eye appeared worse for both signs and symptoms of ocular surface disease. Additionally, I switched him to a hydrogen peroxide disinfection system for advanced cleaning and comfort. To maintain his ocular surface health, the patient performs a daily regimen of eyelid hygiene, uses antihistamine eye drops in the morning and preservative-free artificial tears multiple times a day. (For more on treating dry eye disease, read Practicing Medical Optometry, at bit.ly/KoettingDED . For previous coverage on ocular allergy, read bit.ly/2FRtNWL .)
PROBLEM 2: IMPROPER LENS FIT
The patient was wearing a spherical edge-designed scleral lens that was not the right fit and, thus, appeared to be the main cause of his signs and symptoms: a mild papillary reaction, corneal neovascularization OU and stromal haze OD, explained the photophobia.
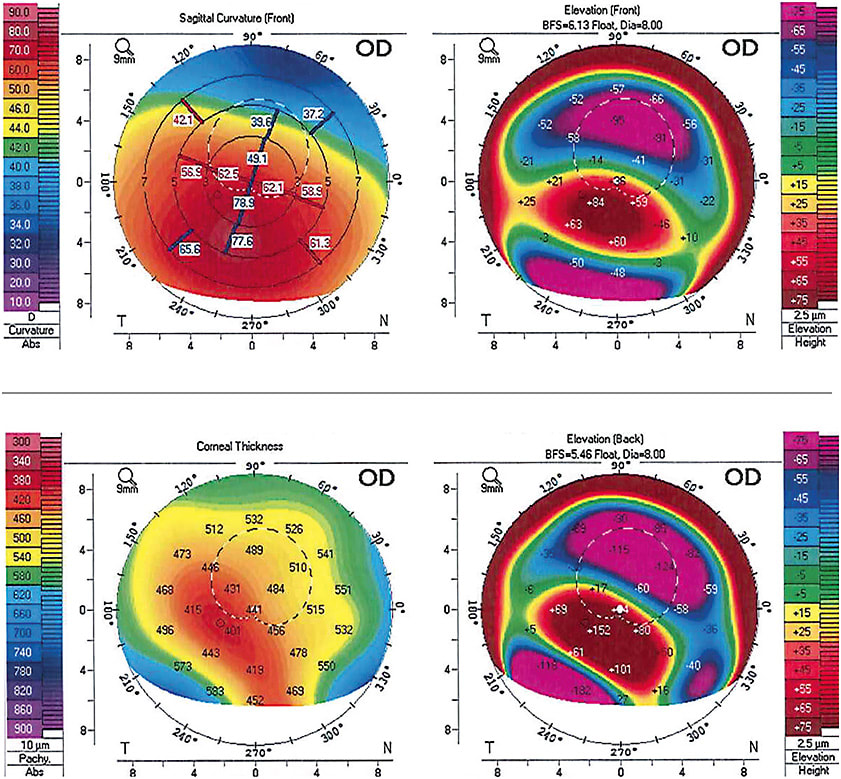
Diagnostic tools: Scleral lens evaluation by slit lamp examination revealed significant blanching and impingement of the inferior conjunctival vasculature, due to a tight fit. Additionally, there was inadequate clearance OU with corneal touch worse OD than OS. Corneal tomography confirmed inferior steepening with high keratometry readings (astigmatism): The patient required a high sagittal depth scleral lens to sufficiently vault the cornea all day.
Corneal surface imaging is important to perform prior to a scleral lens fit to visualize the corneal shape and its potential limitations. This imaging is accomplished via a corneal topographer that uses Placido disk images to formulate a topographical map of the anterior corneal surface and a corneal tomographer that uses Scheimpflug technology to formulate maps of the anterior and posterior corneal surfaces.1
Solution: Once the eye was quiet, a custom, high sagittal depth scleral lens with toric peripheral curves was fit.
Due to the patient’s ocular surface history, previous experience with lenses and unique anterior segment shape, he needed a custom solution. If needed, additional information could have been obtained with the help of corneo-scleral profilometry. This technology provides measurements of the cornea and sclera, giving data points over 18 mm, 20 mm or 22 mm in diameter (depending on the system) in multiple gaze positions. One commercially available system can take measurements in up and down gaze positions also, and another does not require the use of fluorescein.
Once all of the data is collected, and the custom lens is acquired from the appropriate laboratory, it is time to put a lens on the eye.
Practice management note: The length of the appointment and required follow-up appointments must be communicated with the patient from the beginning. Many patients are accustomed to going home with contact lenses same day, however that is never the case with scleral lens wearers, and they should be prepared for that. Discussion should be centered around the customization of the lens to the patient’s eye without compromising health.
CLEAR AND COMFORTABLE VISION
The practice of scleral lens fitting is undeniably both an art and science. A successful fit must meet the eye’s metabolic demands, while providing optimal vision and all-day comfort. All things considered, it can be a challenge for even the most experienced practitioner. However, clear and comfortable vision is most definitely achievable. It is crucial for the practitioner to stay up to date on new technology and research to be successful in these instances.
The aforementioned patient wears his scleral lenses all waking hours without discomfort and looks forward to his 6-month scleral lens appointment to ensure a proper fit and optimal ocular surface. OM
Scleral Lens-Fitting Technologies
THE FOLLOWING technologies aid in the fitting of sceral lenses.
Topographers
- TMS-4N (AIT Industries)
- Visionix VX110 Multi-Diagnostic Unit (AIT Industries)
- Visionix VX120 Multi-Diagnostic Unit (AIT Industries)
- Orbscan III (Bausch + Lomb)
- EasyScan (EasyScan USA)
- OPD-Scan III (Marco)
- Medmont meridia (Medmont International)
- Oculus Keratograph 5M (Oculus)
- Aladdin-M (Topcon Medical Systems)
- CA-200F Corneal Analyzer (Topcon Medical Systems)
- CA-800 Corneal Analyzer (Topcon Medical Systems)
- KR 7000P (Topcon Medical Systems)
- Galilei Dual Scheimpflug Analyzer (Ziemer Group)
- Atlas 9000 (Zeiss)
- Zeiss Atlas 992 (Zeiss)
*This list will be updated at optometricmanagement.com .
Anterior Segment Optical Coherence Tomography AS-OCT
- Xephilio OCT-A1 with anterior segment adapter ASA-1 (Canon)
- SL-OCT (Heidelberg Engineering)
- Spectralis (Heidelberg Engineering)
- AngioVue OCT-A with AngioVue Comprehensive or AngioVue Essential (Optovue)
- Avanti Widefield OCT with Corneal Advance (Optovue)
- iVue OCT (Optovue)
- RS-3000 (Nidek)
- Maestro2 (Topcon)
- Triton (Topcon)
- Cirrus (Zeiss)
- Visante OCT (Zeiss)
Corneo-Scleral profilometry
- sMap3D (sMap3D)
- Eaglet ESP (Eye Surface Profiler)
- Pentacam CSP (Cornea Scleral Profile)
REFERENCES
- Greenwald MF, Scruggs BA, Visliel JM, Griener MA. Corneal Imaging: An Introduction. EyeRounds.org . Posted October 19, 2016; Available from: http://EyeRounds.org/tutorials/corneal-imaging/index.htm .




