A look at the measures to take when faced with end-stage dry eye disease
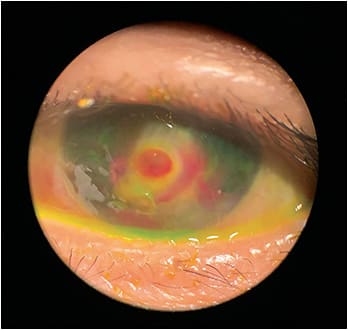
We all have them — those dry eye disease (DED) cases that seem to worsen no matter what we prescribe. Typically, these patients have an underlying systemic disease process, such as Sjögren’s syndrome, Stevens-Johnson syndrome, neurotrophic keratitis, trigeminal neuralgia or limbal stem cell deficiency, to name a few. Thus, these suffering end-stage DED patients often need more aggressive treatment.
Here, I discuss such treatments:
TOPICAL TREATMENTS
I will typically utilize at least one, if not more, of these at the same time:
- Vitamin A ointment. Deficiency of vitamin A is a risk factor for DED, as it impacts the tear’s mucin component and the acinar cells of the lacrimal system.1 It has been used, at bedtime for two to six months, for the treatment of patients who have goblet cell deficiency.1 It can be compounded or obtained online without a prescription.
- Amniotic membranes/drops. Amniotic membranes (AM) protect and nourish the cornea via restorative stem cells. Their use may need to be repeated routinely for our severe DED patients. (For more in-depth information, visit bit.ly/36SSCPY .)
AM cytokine drops work in the same capacity as the membranes, but allow for daily sustained usage. They decrease the clinical signs and symptoms of DED.2 - Autologous serum (AS) drops. These provide cell growth support and migration of the corneal epithelial cells. Recent research reveals symptom relief with AS vs. artificial tears in the short-term.3
- Cenegermin-bkbj. Cenegermin-bkbj ophthalmic solution 0.002% (OXERVATE, Dompé) is a recombinant human nerve growth factor that supports epi-thelial survival/maintenance, tear production and corneal nerve innervation.4 All are needed for our severe DED patients.
THERAPEUTIC LENSES
Protection of the eye’s front surface, reducing eyelid friction and promoting healing can be accomplished utilizing soft or scleral contact lenses. These are used in conjunction with the above topical treatments and all of the less-aggressive DED treatments.
When a soft contact lens is used, it is typically left in place for up to a month, with concurrent use of topical antibiotics.5 This helps to protect the front surface from mechanical rubbing of the eye lids, decreasing potential filament production and helping with pain.6 In patients who have chronic epithelial defects due to severe DED and neurotrophic keratitis, these lenses help to facilitate healing.6
Scleral lenses protect the ocular surface by providing continuous corneal hydration and are often used with other therapies, such as topical corticosteroids.7
SURGERY
When the other options fail, we look to surgery:
- Punctal cautery. This can be used in a patient who has found punctal plugs beneficial but may have trouble keeping them seated in the puncta well, or they create lid apposition.8
- Partial or full tarsorrhaphy. The lid is either partially or fully sutured together, allowing the corneal surface to heal. It can be reversed and opened later with minimal-to-no long-term consequences. Tarsorrhaphy is often recommended for patients at risk for chronic corneal infections, ulcers or perforations.9 With partial tarsorrhaphy, we may also utilize therapeutic lenses and the topical treatments mentioned.
- Conjunctival flap. A flap of conjunctival tissue is placed over the cornea to help re-establish the integrity of the corneal surface, providing metabolic and mechanical support for healing, relieving pain and reducing topical medication usage. Vision will be significantly compromised, but it can be reversed and may or may not need further surgery, such as a limbal stem cell transplantation. When this is performed, however, it is more often not reversed and is the final step for severe DED.
CHEER PATIENTS ON!
Don’t throw in the towel with your severe DED patients. Stop, think outside the box and try one of these mentioned treatments to see whether patients can achieve relief. Regardless, they’ll thank you for your efforts. OM
REFERENCES
- Milner MS, Beckman KA, Luchs JI, et al. Dysfunctional tear syndrome: dry eye disease and associated tear film disorders – new strategies for diagnosis and treatment. Curr Opin Ophthalmol. 2017 Jan; 28(Suppl 1): 3–47. doi: 10.1097/01.icu.0000512373.81749.b7.
- Yeu E, Goldberg DF, Mah FS, et al. Safety and efficacy of amniotic cytokine extract in the treatment of dry eye disease. Clin Ophthalmol. 2019 May 27;13:887-894. doi: 10.2147/OPTH.S203510.
- Pan Q, Angelina A, Marrone M, Stark WJ, Akpek E. Autologous serum eye drops for dry eye. Cochrane Database Syst Rev. 2017 Feb 28;2(2):CD009327.
- Sacchetti M, Bruscolini A, Lambiases A. Cenegermin for the treatment of neurotrophic keratitis. Drugs Today. 2017 Nov;53(11):585-595. doi: 10.1002/14651858.CD009327.pub3.
- Ehlers JP and Shah CP, eds. The Wills Eye Manual Fifth Edition, Wolters Kluwer Health, New York, New York, 2008:15-16.
- Chan WE, Weissman BA. Therapeutic contact lenses. In: Bennett ES, Weissmann BA, (eds). Clinical Contact Lens Practice, Lippincott Williams & Wilkins: New York, New York, 2005: 619-628.
- Harthan JS, Shorter E. Therapeutic uses of scleral contact lenses for ocular surface disease: patient selection and special considerations. Clin Optom (Aukl). 2018; 10: 65–74. doi: 10.2147/OPTO.S144357.
- Wang Y, Carreno-Galeano JT, Singh RB, Dana R, Yin J. Long-term Outcomes of Punctal Cauterization in the Management of Ocular Surface Diseases. Cornea. 2021 Feb 1;40(2):168-171. doi: 10.1097/ICO.0000000000002384.
- Cosar CB, Cohen EJ, Rapuano CJ, et al. Tarsorrhaphy: clinical experience from a cornea practice. Cornea. 2001 Nov;20(8):787-91.




