It’s not the same as dry eye disease
The Tear Film & Ocular Surface Society’s International Workshop on Contact Lens (CL) Discomfort broadly defines contact lens discomfort as reduced compatibility between the contact lens and the ocular environment. Further, the report points to multiple, possible causes related to either the CL itself or the patient’s individual physiological characteristics.1 The signs and symptoms of CL discomfort often masquerade as dry eye disease (DED). Thus, the phrases “contact lens dry eye” or “contact lens-induced dry eye” are more accurate in describing the exacerbation of preexisting DED in a CL wearer.1
Here, I discuss how to differentiate between DED and CL discomfort, and manage CL discomfort.
DIFFERENTIAL DIAGNOSIS
A CL discomfort diagnosis may be made after the patient, who was not previously diagnosed with DED, has tried a reasonable period of adaptation. (This is relative to lens type.) This is one of the reasons to diagnose DED and treat any underlying ocular surface deficiency prior to initiating CL fitting or refitting.
CL discomfort can occur in the presence or absence of visual disturbance. Also, CL patients who complain of “dry eye” but who are asymptomatic when not wearing CLs and who, likewise, exhibit normal findings on tear film and ocular surface evaluation, can be considered to have CL discomfort.
Additionally, CL discomfort may be attributed to material incompatibility (e.g., in the presence of poor anterior lens surface wetting, and/or a less-than-optimal fit or modulus). Thus, a case history and clinical exam are critical for CL material and design selection.
Also, the condition may be diagnosed when ocular signs including, but not limited to, conjunctival hyperemia, meibomian gland changes, and corneal and conjunctival staining are detected.
MANAGEMENT
The following approach has enabled me to effectively manage contact lens discomfort:
- Eliminate the contact lens solution. Prescribe daily disposables, when possible, or prescribe a hydrogen peroxide care system.
- Evaluate lens movement. Don’t prescribe CLs that move excessively (more than 1 mm with blink) or, conversely, cannot be moved with digital manipulation. If there is adequate corneal coverage, consider a steeper base curve. CLs that are too tight will cause visual blur immediately after a blink; loose lenses will clear with the blink.
- Optimize lens diameter. Aim for a approximately 1 mm to 1.5 mm of scleral coverage.2
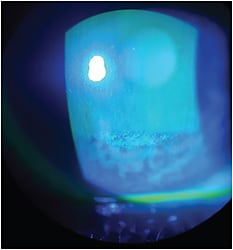
- Monitor the palpebral conjunctiva. Evert the lids at every CL evaluation appointment. Papillae and/or lid-wiper staining implies frictional insult, so a change in material, modulus, and/or edge design should be considered.
- Employ vital dyes. The location and type of staining (i.e., punctate or coalesced) will reveal frictional bearing of the CL, problems related to the blink, or CL and ocular dehydration.
FINAL THOUGHTS
Keep in mind that while oxygen transmissibility is important for corneal health, it has not yet been substantially linked to CL comfort. Modifiable factors, such as lubricity and wettability, may have an impact on CL comfort.
Our goal is to ensure patients can wear their lenses without sensation and for as long as desired or needed. This is accomplished through a detailed patient history and methodical clinical evaluation during each patient encounter. OM
References are available in the online version of this column.




