In the past, optometrists were trained to associate dry eye disease (DED) with menopausal women, advanced age, or chronic auto-immune diseases, such as Lupus, Sjögren’s syndrome, or thyroid disease. The face of DED has changed.
Specifically, the chronic condition now affects all populations, with studies revealing a particular compelling connection between prolonged digital device use (phones/computers) and the propensity for DED.1 Longer screen time has resulted in abnormal TBUT times, tear meniscus height, Schirmer’s and ocular surface disease index (OSDI) scores.2 Who doesn’t use some sort of digital device nowadays?
Something else to consider: 14.1% of adults ages 21 to 49 have DED, and 15.2% of adolescents have DED.3,4
Here, I discuss the common causes of DED in the various age groups and how optometrists can manage these patients’ DED, acknowledging that ODs are not necessarily going to be successful in changing their patient’s DED-causing conditions or behaviors. (See “DED Treatments,” p.21)
THE SILENT GENERATION
Common causes: Born between 1928 and 1945, this generation’s DED is often secondary to advanced age, systemic health conditions (e.g., diabetes, cardiovascular disease, depression), ocular comorbidities (e.g., glaucoma or refractive surgeries), and the use of multiple ocular surface-drying systemic medications, such as anti-depressants.5
The natural aging process is the main contributing factor for DED in this patient population, caused by decreased tear production, lid laxity, conjunctivochalasis, meibomian gland atrophy, and meibomian gland orifice metaplasia (anterior migration of Marx’s line).6
Management: Optometrists managing this generation don’t have a lot of control over the medications these patients use daily, however, they can propose a daily treatment plan to help prevent or minimize the symptoms of DED. First, they can conduct a thorough review of systems and the patient’s medication list to identify the drugs and health conditions most likely to disrupt the tear film and cause DED. These include diuretics, antipsychotics, antihistamines, and pain medications. Systemic conditions include diabetes, thyroid disease, and autoimmune diseases. Second, ODs can recommend prophylactic at-home treatments, such as proper daily lid hygiene, cleaning with tea tree oil or hypochlorous lid cleansers, and nightly warm compresses with moist heat for up to 10 minutes, preferably with a heated beaded mask. Also, optometrists can recommend preservative-free artificial tears up to three times per day, as needed, quality daily omega supplements, and monitor the patient’s daily water intake. Third, they can educate the patient and their caregiver on the DED findings, write the treatment plan, and send a detailed letter to the primary care physician, noting the DED diagnosis and the prescribed treatment plan.
Finally, ODs can monitor closely. I typically see my DED patients every four to six months. Topical therapy and advanced treatments are an option as well for this generation if the condition progresses.
DED Treatments
- Artificial tears
- Lid hygiene and care (e.g., scrubs, wipes, sprays masks, warm compresses, tea tree oil application/okra-based lid scrub)
- Environmental changes (e.g., moving away from temperature vents)
- Behavior changes (e.g., blink breaks from digital device use)
- Omega-3/6 supplementation
- Corticosteroids
- Anti-inflammatory agents
- Autologous serum eye drops
- Meibomian gland expression
- In-office treatment devices (See p.33)
- Scleral contact lenses
- Amniotic membrane
- Punctal plugs
- Ophthalmic inserts
- Neuromodulation Therapy
THE BABY BOOMERS
Common causes: This generation, born between 1946 and 1964, share aging with the Silent Generation as a risk factor for their DED. In my clinical experience, systemic comorbidities, such as type 2 diabetes and menopause/peri-menopause, are most likely the major contributing factors for their DED.
Regarding diabetes, studies reveal 39% of Baby Boomers are obese, with 16% diagnosed with type 2 diabetes.7 While optometrists are trained to monitor diabetic patients for retinopathy and macular edema, the ocular manifestation of DED can be overlooked. In fact, one study indicates that 53% of patients who have either diabetes or borderline diabetes reported clinically significant DED.8 What’s more, The Beaver Dam Eye Study shows that 20% of patients who have diabetes had dry eye symptoms.9
In reference to menopause/peri-menopause, it is believed that the body produces less estrogen, progesterone, and androgen hormones. Research reveals a reduction in the androgen hormone negatively affects both the lacrimal gland and meibomian glands.10 Lower androgen levels incite an inflammatory change in the lacrimal gland, resulting in less basal tear production (aqueous-deficient dry eye).11 Dysfunctional meibomian glands cause less meibum secretion, resulting in increased tear film evaporation (evaporative DED).
Management: Optometrists don’t have a lot of control over what a primary care physician or rheumatologist prescribes for these patients. I recommend screening every patient who has diabetes, as well as menopausal/peri-menopausal patients (ages 45 to 55) for DED with an in-office questionnaire, such as the OSDI or Standard Patient Evaluation of Eye Dryness questionnaire. If the patient is symptomatic, I suggest performing further DED testing and treating as necessary. If the patient is asymptomatic, I recommend educating the patient on the connection between DED and their condition. Optometrists can prescribe a specific type of preservative-free tear twice per day, discuss the importance of daily lid hygiene, review makeup application and removal habits. Lastly, ODs can advise the patient to return to their office immediately if they experience consistent symptoms associated with DED (redness, burning, grittiness, or blurry vision).
In my clinical experience with this patient population, if tolerated, this demographic responds well to daily topical prescription DED drugs, such as an immunomodulator, to reduce inflammation and regulate basal tear secretion.
THE ALPHABET GENERATIONS
Common cause: Generation X (born 1965 to 1980), Millennials (born 1981 to 1996), Generation Z (born 1997 to 2012), and Generation Alpha (born 2013 to 2025) all share two common behaviors that significantly increase their risk for DED: excessive digital screen time and unregulated beauty trends.
Regarding excessive digital screen time, according to Statista, close to half of Americans spend five to six hours on their phone daily, not including work-related smartphone use. Additionally, 22% say they spend three to four hours on average on their phone daily. Further, most Americans say they use YouTube and Facebook, while the under-30 crowd flock to Instagram, Snapchat, and TikTok, according to the Pew Research Center,
Studies reveal that excessive device or computer use negatively impacts the normal blink rate (12 to 15 per minute), reducing it by nearly 50%.12 Changes in the blink rate may cause ocular discomfort symptoms, such as redness, burning, or excessive tearing, more than likely triggered by a lack of adequate tear distribution.12 Boom! Here comes DED!
In reference to unregulated beauty trends, many can be harmful to the ocular surface, causing DED and/or exacerbating symptoms by disrupting the tear film. Many trends involve applying foreign materials and chemicals to the lid and lash margin. These include lash lifts, permanent eyeliner, retinoid-based skin care, cosmetic products that contain high levels of toxic ingredients, applying makeup on the waterline, glitter eye shadow, and individual lash extensions, along with poor lash hygiene habits by patients. In my clinical experience, many of these harmful trends (retinoid creams and permanent tattoo eyeliner) clog or destroy the meibomian glands, or they disrupt the normal biofilm (lash extensions), resulting in blepharitis and MGD.
Management: When it comes to excessive digital screen time, ODs should educate both young and older patients on the 20-20-20-blink rule: every 20 minutes, look 20 feet away for 20 seconds, then blink. Also, optometrists should advise these patients to make sure their computer monitor is eye level or slightly below to minimize the risk of DED symptoms throughout the workday. Lastly, ODs can prescribe an OTC preservative-free artificial tear to use during the day, for ocular dryness or discomfort. I explain to my patients, “We use ChapStick as needed to moisturize our lips. Why not do the same for our eyes?”
For those patients interested in makeup, optometrists should provide sound advice on the aforementioned harmful cosmetic trends — Think Dirty, INCI Beauty and EWG’s Skin Deep are downloadable resources. Additionally, optometrists can recommend safe alternatives, such as makeup from Eyes Are the Story, Twenty/Twenty Beauty, We Love Eyes, OpulanceMD Beauty, and Oculaire Skincare. ODs may even want to partner with these industry beauty brands to offer wholesale or online purchase opportunities to help increase patient awareness. (See “Steps for Managing DED Regardless of Patient Population,” p.24.)
Steps For Managing DED Regardless of Patient Population
THE FOLLOWING ARE APPLICABLE TO ALL DED PATIENTS, DESPITE THEIR AGE:
- Screen. In my practice, for example, we start screening patients age 12 and older during the pretesting process. Specifically, my technician begins this process by employing the Ocular Surface Disease Index (OSDI) questionnaire and asking probing questions, such as, “Do your eyes feel dry or irritated?” “Do you put tears in your eyes during the day?”
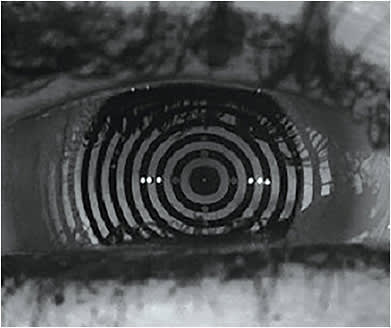
- Perform diagnostic testing. This commences when the data reveals suspicion for DED. In addition to using vital dyes (sodium fluorescence, rose bengal, or lissamine green) to assess TBUT and cornea/conjunctival staining, and Schirmer’s strip testing, a more definitive diagnosis can be achieved via measuring tear volume, tear osmolarity, examining the meibomian glands, meibomian gland expression, and MMP-9 testing. (See “Determine the Root Cause of Dryness,” at bit.ly/DEDDiagnosis .)
- Educate. I use the same analogy for all patients: “For you to see clearly and comfortable, your eyes must stay moist and hydrated. The tear film is responsible for keeping your eyes moist and hydrated. I like to call the tear film your ‘eyeball lotion.’ The tear film is made up of several components, including water, lipids, and mucous. If the quality of your tear film is not optimal, your eyes won’t stay moist and hydrated. If the tear film stays imbalanced, inflammation will ‘set up’ in the eyes, causing frequent burning, redness, grittiness, and blurry vision. It is important for us to examine the quality of your tear film to determine the root cause of your discomfort and devise a customized treatment plan.”
- Provide treatment documentation. Research shows that patients immediately forget over 40% of medical information and doctors’ instructions as soon as they leave the office.13 In addition to taking the time to verbalize the treatment plan, optometrists should give patients a treatment plan document comprised of what to take, when to take it, who to contact for additional questions or concerns, and how to reorder supplements and products. In my practice, every patient leaves the office with clear, hand-written instructions, follow-up recommendations, and a coupon or discount code to reorder products. My technician quickly reiterates my instructions, dispenses recommended products, and schedules the patient accordingly.Treating DED can take up a lot of chair time unless optometrists have a process in place to help patients remember their customized treatment plan and mitigate office “call-backs” regarding instructions. ODs can offer online chat or short message service communication to quickly answer patient questions or concerns.
While all patients are different, I find that patients of all ages can experience mild episodic redness, gritty sensations and burning, typically exacerbated by environmental changes, cosmetic habits, or excessive amounts of device time. Usually, I prescribe a “foundational” drug-free home treatment plan: tea tree oil-based lid cleansers or hypochlorous spray, warm compresses once to twice per week, preservative-free artificial tears to use as needed (maximum three times per day), a daily oral omega supplement and, lastly, recommend a clean makeup and skin care regimen. Symptomatic patients with an abnormal OSDI score are schedule back in two weeks for a full DED workup.
PREPARE FOR REJECTION
Despite our best efforts, ev-ery patient will not accept the prescribed treatment plan. But if given alternatives, the chance of getting patients to change their behaviors can increase. Patient education is the OD’s superpower, as an educated patient feels empowered to make better decisions. The face of DED has changed, but we are at the forefront of diagnosis and effective management. OM
REFERENCES
- Mehra D, Galor A. Digital Screen Use and Dry Eye: A review. Asia Pac J Ophthalmol. 2020 Dec;9(6):491-497. doi: 10.1097/APO.0000000000000328.
- Akib MN, Pirade SR, Syawa SRl, Fauzan MM, Eka H, Seweng A. Association between prolonged use of smartphone and the incidence of dry eye among junior high school students. Clinical Epidemiology and Global Health. 2021. ISSN 2213-3984 https://doi.org/10.1016/j.cegh.2021.100761 .
- Paulsen, AJ, Cruikshanks KJ, Fischer ME, et al. Dry eye in the beaver dam offspring study: prevalence, risk factors, and health-related quality of life. Am J Ophthalmol. 2014;157(4): 799-806. doi: 10.1016/j.ajo.2013.12.023.
- Ayaki M, Kawashima M, Uchino M, Tsubota K, Negishi K. Gender differences in adolescent dry eye disease: a health problem in girls. Int J Ophthalmol. 2018 Feb 18;11(2):301-307. doi: 10.18240/ijo.2018.02.20.
- Sharma A, Hindman HB, Aging: A predisposition to dry eyes. J Ophthalmol. 2014;2014:781683. doi: 10.1155/2014/781683.
- de Paiva, CS. Effects of Aging in Dry Eye. Int. Ophthalmol Clin. 2017;57(2):47-64. doi: 10.1097/IIO.0000000000000170.
- King DE, Matheson E, Chirina S, Shankar A, Broman-Fulks J. The status of baby boomers’ health in the United States: the healthiest generation? JAMA Intern Med. 2013 Mar 11;173(5):385-6. doi: 10.1001/jamainternmed.2013.2006.
- Hom, M, De Land P.Self-reported dry eyes and diabetic history. Optometry. 2006 Nov;77(11):554-8. doi: 10.1016/j.optm.2006.08.002.
- Klein R, Klein BE, Linton KL, De Mets DL. The Beaver Dam Eye Study: visual acuity. Ophthalmology. 1991;98(8):1310-5. doi: 10.1016/s0161-6420(91)32137-7.
- Truong S, Cole N, Stapleton F, Golebiowski B. Sex hormones and the dry eye. Clin Exp Optom. 2014;97(4): 324-36. doi: 10.1111/cxo.12147.
- Arita R, Itoh K, Inoue K, Amano S. Noncontact infrared meibography to document age-related changes of the meibomian glands in a normal population. Ophthalmology. 2008;115(5):911-5. doi: 10.1016/j.ophtha.2007.06.031.
- Abusharha, AA. Changes in blink rate and ocular symptoms during different reading tasks. Clin Optom (Auckl). 2017;9:133-138. doi: 10.2147/OPTO.S142718.
- Kessels, RPC. Patients’ memory for medical information. J R Soc Med. 2003 May;96(5):219-22. doi: 10.1258/jrsm.96.5.219.




