As optometrists, we know all too well that the proper management of our contact lens (CL) patients involves the consistent, careful, and methodical evaluation of patient expectations, CL performance, and ocular health via the CL exam.
A problem arises, however, when we use the term routine to label or describe the CL exam. The reason: Routine sends the message to patients that the CL exam isn’t a priority, causing them to question its need. Also, I think we should keep in mind that no CL patient encounter is ever “routine.” Whether applied to the most challenging or least complex case of wear, the OD’s expertise and knowledge are ever present and critical in meeting the highest standards of care. CL-wearing patients need to know this.
I have found that communicating the value and importance of both the baseline and periodic (not routine) CL exam fosters patient compliance to their prescribed wear and care regimen, improves clinical outcomes, and engenders greater patient loyalty to a practice. (See “More on Contact Lenses,” p.38.)
My approach to differentiating and highlighting the significance of the CL exam for patients involves these five areas:
1 APPOINTMENT SCHEDULING
Effective communication about the importance and distinction of the CL exam starts here and is tailored to whether the patient is new or a returning patient, and whether the patient is a current CL wearer.
“Shall we have the doctor assess your potential as a contact lens wearer, in addition to analyzing your eye health and vision”? is posed to all new and current primary care patients.
Our team will, likewise, inquire of all current wearers whether they are experiencing any changes, asking “are you experiencing any changes in vision or comfort”? While informing patients that they should come in wearing their CLs, we are further able to emphasize that the CL evaluation is a distinct and separate part of the exam by adding “your contact lens evaluation will be performed first.”
2 FEE STRUCTURE
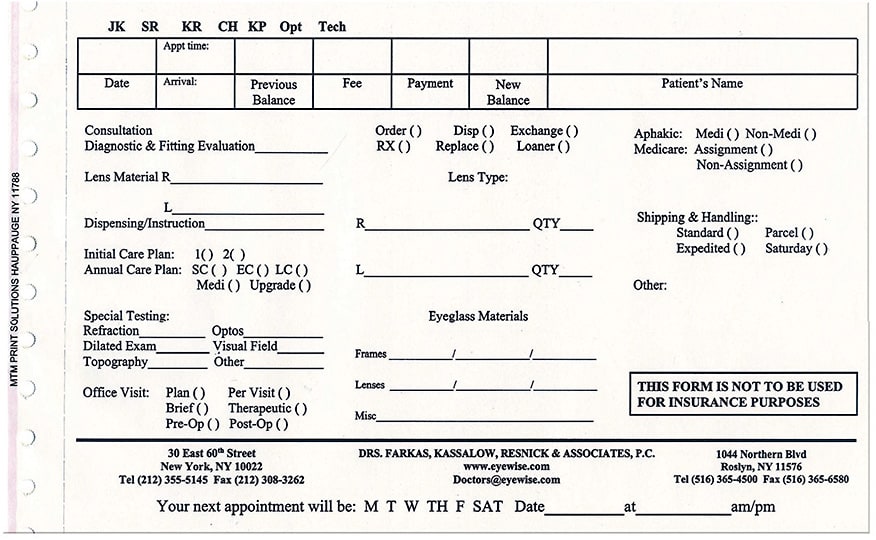
I have discovered that having a dedicated and itemized fee schedule that separates the CL exam’s professional fees from the related special testing and material fees is critical to the successful administration and communication of my clinical approach, as it informs patients of what the CL exam entails. (See image on p.38.) This, in turn, supports the costs associated with said exam. I think it’s important to note that no one is going to be amenable to paying something that they view as an additional, unnecessary fee.
Where I practice, we itemize our fee structure to include the diagnostic evaluation, the insertion training, material fees, and follow-up care. We avoid the word “fitting,” as it has a more limited connotation than the comprehensive evaluation of our patients’ visual and physiologic needs. These needs guide our selection of lens material and design, in addition to assuring optimum on-eye CL performance.
3 PATIENT SCREENING
At each CL exam, I provide the patient with a modified Standardized Patient Evaluation of Eye Dryness, or SPEED, questionnaire to quickly identify patients who have symptoms of CL discomfort. Specifically, I ask them to respond to the questions twice: once per-taining to their experiences without CL wear and the other with CL wear.
While this action step takes a few extra minutes, I find that it goes a long way in demonstrating that CL wear imparts another level of complexity inherent to this exam and helps guide my decision making regarding the need for related clinical testing.
4 PRE-TESTING AND AUXILIARY TESTING
After the patient completes the SPEED survey, they undergo an auto-refraction over their CLs (or without CLs, if the patient is new to wear).
Next, the technician briefly chats with the established CL wearer to ascertain whether that patient has experienced any acute changes in comfort or vision. Based on the answers, the technician briefly discusses related new CL technologies.
For example, should an established CL wearer mention difficulty reading, the technician responds, “We have lens designs that can restore your focusing flexibility; I will mention this to the doctor for you, so that this will be carefully evaluated.”
The pre-exam discussion may also elicit auxiliary testing, such as corneal topography and axial length — specialized testing not part of the comprehensive eye exam — and impresses upon the patient that additional diagnostics play a role in CL selection, design, and follow-up care.
5 METICULOUS CLINICAL EVALUATION
As I conduct each part of the clinical evaluation, which is comprised of VA, over-refraction, slit lamp exam, with and without CLs, and diagnostic meibomian gland expression, I describe the purpose of the instrumentation used and vital dyes, the structures I am looking at and why, as well as my observations.
For example, while using a meibomian gland expressor to perform diagnostic meibomian gland expression, I explain to patients that I am assessing the health of the glands, which provide an important layer of the tears. Additionally, I relate that I am evaluating tear film integrity both in the presence of the CL and after CL removal to monitor ocular surface health, consistency of vision, and to ensure optimum comfort.
Additionally, while examining the cornea, I explain to CL-wearing patients that ocular health changes, such as neovascularization, corneal staining, and edema, may be asymptomatic findings, reemphasizing the fact that the CL exam should not be viewed as routine.
I conclude the CL exam by relating my findings back to any specific patient complaints, clinical findings, or challenges and laying out an action plan specific to that patient.
EDUCATION WANTED
In talking to colleagues and in reading related articles, it appears that if ODs and their staff members don’t take the time to educate patients about the value of the CL exam, patients will view it as an added and unnecessary fee. By using the five areas described above, however, this can be avoided, while showing patients the immense benefit they receive through these optometrist-run exams. OM
MORE ON CONTACT LENSES


HOW CAN ODs RETAIN CONTACT LENS SALES?

HOW CAN OPTOMETRISTS FIT MORE MULTIFOCAL CONTACT LENSES?

HOW CAN ODs DETERMINE FIT SETS AND THE AMOUNT TO KEEP ON HAND?





