The optometrist’s role before and after corneal collagen cross-linking
Although historical estimates place the incidence of keratoconus (KCN) at approximately 1 in 2,000 in the general population, a more recent meta-analysis of 29 articles spanning 15 countries, revised this to 1.38 per 1,000 in the general population.1,2
Fortunately, advances in contact lens (CL) technology enable optometrists to manage the visual complications of KCN, namely corneal ectasia. In fact, a retrospective chart analysis of over 2,800 eyes shows that patients who wear scleral or RGP CLs have almost one-fifth the risk of undergoing keratoplasty.3 Scleral CLs, in particular, can significantly reduce the need for corneal transplants in severe KCN.4
With the advent of corneal collagen cross-linking (CXL), however, the optometrist’s role goes beyond contact lens fitting for visual rehabilitation. The OD, often the first to diagnose and detect corneal ectasia, has the opportunity and responsibility to evaluate and appropriately refer patients for this proven and effective procedure. (See “CXL: An Overview,” p.50.)
BEFORE CROSS-LINKING
When coordinated scheduling with the surgeon permits, ODs should have current CL wearers discontinue wear a week or two prior to the surgical consultation leading up to the actual procedure. Doing so allows for a pre-procedure topographical and corneal thickness analysis free from the mechanical and physiological effects of CL wear, which can negatively affect the pre-operative corneal thickness evaluation.
In cases in which this is not possible and CL wear needs to be resumed after pre-procedure measurements and before surgery, CLs should be removed 3 days prior to treatment.
AFTER CROSS-LINKING
While confocal microscopy shows that epithelial thickness can take 3 to 6 months to return to normal after epi-off CXL, patients’ often need more immediate visual rehabilitation.5
Optometrists should base initiation or resumption of CL wear upon the method of CXL, the post-procedure refractive stability, epithelial integrity, and type of CL being fit.
In my clinical experience, the ideal time to consider fitting or refitting is 2 weeks post epi-on CXL and 4 to 6 weeks after epi-off CXL. In all cases, postop steroid drops will have been discontinued, as they increase the risk of infection and are contraindicated in contact lens wear.
A surprised patient can be an unhappy patient. Therefore, ODs should advise postop CL wearers that prescription or fit alterations may be needed over the next 6 to 12 months, as refractive changes can be linked with the corneal remodeling associated with CXL recovery. I have found that a practical approach in managing current CL wearers is to re-evaluate them postop with the CLs they wore prior to surgery and modify as necessary.
In terms of CL choice, I have discovered that conventional soft CLs may be fit in cases of acceptable best-corrected spectacle vision with repeatable refraction after complete corneal healing. In patients who have irregular astigmatism and more advanced corneal ectasia, the optometrist should consider a specialty design soft lens, hybrid, or scleral lens. Conventional soft lenses will conform to the irregularity rather than mask it, failing to provide optimal vision. As scleral lenses completely vault the cornea (and are, therefore, less likely to require modification), they may be fit and worn sooner postop than lenses that rest on the cornea.
CXL: AN OVERVIEW
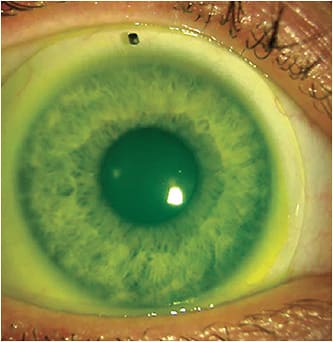
Corneal collagen cross-linking (CXL) leverages oxidation reactions to form bonds between collagen fibrils, providing the ability to alter the natural history of KCN by slowing or stopping its progression.5 The two types of CXL are the epi-off (FDA approved) and the epi-on. The former involves epithelial debridement.
MAKING A DIFFERENCE
With earlier detection of corneal ectasia and timely referral for CXL, in addition to the optometrist’s expert management with CLs, ODs can now even more favorably impact the visual outcomes and quality of life of patients who have KCN. OM
References:
1. Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42(4):297-319. doi: 10.1016/s0039-6257(97)00119-7.
2. Hashemi H, Heydarian S, Hooshmand E, et al. The Prevalence and Risk Factors for Keratoconus: A Systematic Review and Meta-Analysis. Cornea. 2020;39(2):263-270. doi: 10.1097/ICO.0000000000002150.
3. Ling JJ, Mian, SI, Stein JD, Rahman, M, Poliskey J, Woodward, MA.
Impact of Scleral Contact Lens Use on the Rate of Corneal Transplantation for
Keratoconus. Cornea. 2021 Jan;40(1):39-42. doi: 10.1097/ICO.0000000000002388.
4. Koppen C, et al, Scleral Lenses Reduce the Need for Corneal Transplants in Severe Keratoconus. Am J Ophthalmol. 2018;185:43-47. doi: 10.1016/j.ajo.2017.10.022.
5. Mazzotta C, Hafezi F, Kymionis G, et al. In Vivo Confocal Microscopy after Corneal Collagen Crosslinking. Ocul Surf. 2015;13(4):298-314. doi: 10.1016/j.jtos.2015.04.007.
6. Mohammadpour M, Masoumi A, Mirghorbani M, Shahraki K, Hashemi H. Updates on corneal collagen cross-linking: Indications, techniques and clinical outcomes. J Curr Ophthalmol. 2017;29(4):235-247. doi: 10.1016/j.joco.2017.07.003.eCollection 2017 Dec.




