Identify the qualitative features linked with glaucomatous optic neuropathy
After talking with a patient about their recent diagnosis of glaucoma and, subsequently, thinking about it more, the patient wisely asked, “What does glaucoma look like? Is there anything else it could be?”
Such an insightful question brings us to the foundation of all glaucoma care — and something that is “…essential in the management of glaucoma…and…the most common reason for raising a suspicion of glaucoma.”1 — a systematic evaluation of the optic nerve.
Here’s a long answer to this patient’s short question.
LOOKING BACK
Since the relationship between elevated IOP and cup-to-disc ratio (CDR) was first described over four decades ago,2 the CDR has been used as a method to determine whether someone has glaucoma. Unfortunately, and because there is significant overlap between normal and glaucomatous CDRs (similar to IOP levels), such nondescriptive, quantitative measurements have resulted in both the over- and under-diagnosis of glaucoma. CDR is not glaucoma.
Fortunately, and thanks to several key, major-scope articles3-8 over the years, our understanding and recognition of glaucomatous optic nerve damage has been redefined and refined. As a result, these wells of wisdom have helped us better understand and appreciate the qualitative features associated with glaucomatous optic neuropathy, with less and less emphasis on CDR values.
HERE AND NOW...
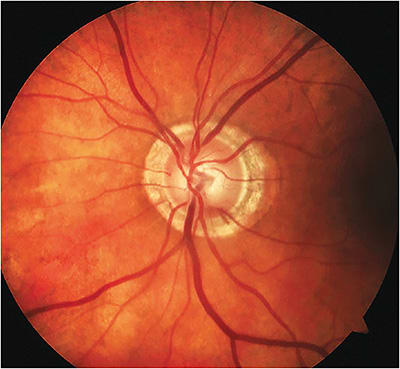
Without any extra cost to the practice, and with immeasurable profit to our patients, what are the qualitative features that we should look for and use for diagnosis? Among other qualitative factors, such as the presence of a glaucomatous disc hemorrhage that we will observe, here is a time-tested triad:9-11
- Diffuse or focal neuroretinal rim narrowing/notching, especially within the inferior temporal or superior temporal sectors. In other words, the inferior temporal and superior temporal sectors are target areas in glaucoma and, therefore, represent some of the earliest signs of glaucomatous optic neuropathy. Such preferential rim loss, in the context of the size of the optic nerve, is even more concerning when there is inter-eye asymmetry, and it will surely lead to correlating VF defects if the resulting rim-to-disc ratio (RDR) is zero.Pro Tip: If we look inferiorly and superiorly every time, we will catch most cases of early glaucoma. In the absence of pallor, neuroretinal rim thinning is glaucoma.
- Diffuse or localized abnormalities of the parapapillary retinal nerve fiber layer (RNFL) pattern, especially within the inferior temporal or superior temporal sectors, as noted above. With diffuse thinning of the RNFL, we will note corresponding increased vessel clarity.Pro Tip: In the absence of neuroretinal rim pallor and/or retinal vascular occlusive disease, diffuse or local RNFL pattern loss is glaucoma.
- Disc hemorrhages. Glaucomatous disc hemorrhages are literally red flags strongly associated with progressive neuroretinal rim thinning and RNFL loss, especially in the inferior temporal and superior temporal sectors.Pro Tip: When associated with preferential glaucomatous structural loss in these locations, and in the absence of retinal vascular or vitreous diseases, flame-shaped hemorrhages are a sign of glaucoma.
THE DEFINITIVE TRIAD
Simply look for this triad of “…characteristic structural changes of the optic nerve…”12 as outlined above. By focusing on such qualitative features, more than quantitative CDR values, we will be able to diagnose glaucoma earlier and detect disease progression sooner. This is glaucoma. OM
References:
1. Sihota R, Sidhu T, Dada T. The role of clinical examination of the optic nerve head in glaucoma today. Curr Opin Ophthalmol. 2021;32(2):83-91. doi: 10.1097/ICU.0000000000000734.
2. Armaly MF, Sayegh RE. The cup-disc ratio. The findings of tonometry and tonography in the normal eye. Arch Ophthalmol. 1969;82(2):191-6. doi: 10.1001/archopht.1969.00990020193008.
3. Kirsch RE, Anderson DR. Clinical recognition of glaucomatous cupping. Am J Ophthalmol. 1973;75(3):442-54. doi: 10.1016/0002-9394(73)91153-7.
4. Jonas JB, Budde WM, Panda-Jonas S. Ophthalmoscopic evaluation of the optic nerve head. Surv Ophthalmol. 1999;43(4):293-320. doi: 10.1016/s0039-6257(98)00049-6.
5. Broadway DC, Nicolela MT, Drance SM. Optic disk appearances in primary open-angle glaucoma. Surv Ophthalmol. 1999;43 Suppl 1:S223-43. doi: 10.1016/s0039-6257(99)00007-7.
6. Spaeth GL, Henderer J, Liu C, et al. The disc damage likelihood scale: reproducibility of a new method of estimating the amount of optic nerve damage caused by glaucoma. Trans Am Ophthalmol Soc. 2002;100:181-5; discussion 185-6.
7. Fingeret M, Medeiros FA, S Remo, Weinreb RN. Five rules to evaluate the optic disc and retinal nerve fiber layer for glaucoma. Optometry. 2005 Nov;76(11):661-8. doi: 10.1016/j.optm.2005.08.029.
8. Spaeth GL, Lopes JF, Jun AK, Grigorian AP, Henderer J. Systems for staging the amount of optic nerve damage in glaucoma: a critical review and new material. Surv Ophthalmol. 2006 Jul-Aug;51(4):293-315. doi: 10.1016/j.survophthal.2006.04.008.
9. Primary Open Angle Glaucoma Preferred Practice Pattern – American Academy of Ophthalmology p 49.
10. American Optometric Association. Optometric Clinical Practice Guideline. Care of the Patient with Open Angle Glaucoma. Page 79. https://www.aoa.org/AOA/Documents/Practice%20Management/Clinical%20Guidelines/Consensus-based%20guidelines/Care%20of%20the%20Patient%20with%20Open%20Angle%20Glaucoma.pdf. Accessed Oct.6, 2022.
11. Budde WM, Jonas JB, Martus P, Gründler AE. Influence of optic disc size on neuroretinal rim shape in healthy eyes. J Glaucoma. 2000;9(5):357-62.
doi: 10.1097/00061198-200010000-00003.
12. Song BJ, Caprioli J. Measuring Glaucoma Progression in Clinical Practice in Glaucoma – Medical Diagnosis and Therapy. Elsevier Limited 2015. Chapter 23:268-276.




