Soft contact-lens-caused red eye is a reason for dropping out of soft contact lens wear, due to its appearance and accompanying symptoms. In fact, 5% of those who drop out of contact lens wear cite red eye as the reason.1 What’s more, close to 50% name discomfort as a reason for dropping out, and etiologies of the discomfort can also cause red eye.1
Here, I discuss the main reasons for soft contact-lens-caused ocular redness and how to resolve them, so patients can return to enjoying the benefits of contact lens wear. It must be noted that the resolution of the signs and symptoms of this common condition begins with the temporary discontinuation of lens wear for all the etiologies discussed.
TIGHT-FITTING OR DEFECTIVE LENS
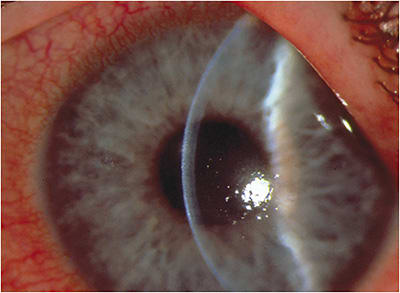
Diagnosis. If the contact lens does not move with the blink and the optometrist is unable to move the lens with their finger, in the absence of any signs of allergy, infection, or complication, a tight-fitting lens is likely the culprit for conjunctival hyperemia. Or upon slit lamp exam, if the contact lens has a tear or chip, this could also be causing the patient’s irritation and ocular redness.
Initially, a patient may not know that the lens is tight. However, over time, the patient will feel lens discomfort or dryness — particularly toward the end of the lens-wearing day. (This can occur alone or in combination with contact lens solution sensitivity, which is discussed below.)
Treatment. For a patient in a tight-fitting lens, I suggest refitting them in a different lens material and/or flatter curvature and instructing them to decrease their contact lens-wearing time, as lenses tighten as the day goes on.2,3 In general, high-water content lenses tighten as the water evaporates from the lens. I switch these patients to a silicone hydrogel lens, which, in general, has a lower water content — one reason that the lens may move more with the blink. (If an anterior chamber reaction is present, I recommend considering prescribing a topical cycloplegic, such as homatropine or scopolamine, bid to tid. Generally, no more than a week of treatment is needed.)
Regarding a defective lens, I instruct the patient to simply discard the contact lens, then I re-educate them on proper lens care and replacement. While patient dependent, I may discuss that long fingernails and catching the lens edge while closing the contact lens case are common causes for a lens rip or chip, though in rare instances, the lens may come out of its vial or blister package this way. If the broken lens created a corneal superficial punctate keratitis, I recommend treating it with topical artificial tears (optimally non-preserved) and adding a topical antibiotic drop (tid to qid) if moderate-to-severe. The artificial tears promote healing, while the antibiotic prevents infection. In most cases, the cornea should be sufficiently healed within one week to discontinue both types of ophthalmic drops.
ALLERGIC CONJUNCTIVITIS/LENS DEPOSITION
Diagnosis. Allergic conjunctivitis presents as bulbar conjunctival hyperemia, inflammation of the bulbar and/or palpebral conjunctiva, and papillae of the upper and/or lower tarsal plates; it is typically bilateral. Patients will likely complain of itching and a watery discharge; I have found most cite a history of allergies. The allergic reaction may be due to pollutants or allergens deposited on the lens.4
Treatment. For allergic conjunctivitis, I recommend eliminating exposure to the offending allergen, if known, and then prescribing topical antihistamines with a mast cell stabilizer — now available OTC- qd to bid), or a mild steroid ophthalmic suspension qid. (I suggest selecting a steroid less likely to cause an increase in IOP, and to measure IOP.) I recommend having the patient taper the steroid at the end of therapy, which is typically one to four weeks.
Regarding lens deposition, I suggest asking the patient at every visit exactly how they are caring for their lenses and how frequently they are replacing them.
If their answer reveals non-compliance as the cause of the lens deposition, I re-instruct the patient on how to clean and disinfect their lenses properly.
If, however, the patient appears compliant with their contact lens care and wear schedule and is simply prone to quick and heavy lens deposition, I recommend refitting the patient in a different contact lens material or prescribing a daily disposable modality.
GIANT PAPILLARY CONJUNCTIVITIS
Diagnosis. Papillae and hyperemia of the upper tarsal plates is seen upon everting the eyelids, and there may be a slight ptosis, if the giant papillary conjunctivitis (GPC) is severe. Additionally, mucous strings may be present (if not seen on the cornea, look at the lower tarsal plate), and the contact lens may decenter up, as the papillae can grab the lens. Also, the lens may be deposited and/or move excessively. While GPC is an inflammatory allergic reaction that is a type 1 and type 4 hypersensitivity reaction, it can also occur from the physical rubbing of a contact lens.
The symptoms of GPC are increased lens awareness, decreased wearing time, foreign body sensation after lens removal, ocular itching, and/or blurring of vision. The latter is due to either lens deposition or lens decentration.
Treatment. Because GPC is highly associated with a deposited soft contact lens, I recommend re-educating the patient on the importance of compliant lens wear and care, and refitting them into a more frequently replaced lens modality, such as a daily disposable, which will limit lens deposition. Additionally, I suggest prescribing an antihistamine-mast cell stabilizer qd to bid topically, or a topical steroid qid, if clinical signs and symptoms are moderate-to-severe. Further, I recommend following up in one week post-prescription, with the understanding that the condition may take up to one month or more to resolve. Finally, I suggest measuring IOP at every visit while the patient is using the steroid ophthalmic suspension.
SOLUTION HYPERSENSITIVITY AND TOXICITY
Diagnosis. Allergic, delayed hypersensitivity reactions to multipurpose solution appear as conjunctival hyperemia and edema affecting the eye(s) wearing the lens, typically in patients who elect to switch solution brands away from what was prescribed. The symptoms of solution hypersensitivity are ocular itching, watering, and discomfort.
In addition, conjunctival hyperemia, tearing, epiphora, chemosis, and/or superficial punctate keratitis can be seen in patients who rewet the eye or rinse their lens with hydrogen peroxide straight from the care system bottle. (As a warning, all major ophthalmic hydrogen peroxide manufacturers utilize a red-colored dropper tip on the bottle.) The symptoms of this are burning, stinging, and photophobia.
Treatment. For solution hypersensitivity, I recommend discussing with patients the importance of using the prescribed solution, citing that generic brands, for example, are often comprised of older formulations that do not employ the latest technologies in safety or wettability. Additionally, I suggest re-educating the patient on the proper wear and care schedule, explaining that deposited contact lenses can bind some preservatives, which can create hypersensitivity.
Regarding hydrogen peroxide solution toxicity, I recommend a thorough in-office rinsing of the ocular surface with saline, ocular wash, or artificial tears. Then I suggest at-home treatment for the patient, which includes the utilization of non-preserved artificial tears at least four times per day. This should facilitate resolution of the keratitis within 24 to 48 hours.
DRY EYE DISEASE
Diagnosis. A contact lens splits the tear film into pre- and post-tear layers, exacerbating dry eye signs and symptoms. Dry eye disease (DED) appears clinically as a decreased (less than 0.25 mm) tear meniscus height, reduced (below 10 seconds) tear break-up time, poor-quality tears, staining of the cornea and conjunctiva, meibomian gland dysfunction, and corneal and/or conjunctival epithelial cell compromise; the bulbar conjunctival hyperemia can range from mild to severe.
The symptoms of soft lens-caused DED are ocular dryness, grittiness, burning, stinging, and irritation, often intensifying as the day wears on. Additionally, these patients will report their lenses are less comfortable at the end of the day as compared with the beginning.
Treatment. Non-preserved artificial tears, lid hygiene, environmental changes, blink breaks, omega supplementation, topical soft steroids, anti-inflammatory agents, serum eye drops, meibomian gland expression, in-office treatment, scleral contact lenses, punctal plugs, ophthalmic inserts, neuromodulation therapy, or amniotic membranes can keep DED at bay.
Lastly, instilling a drop of non-preserved artificial tears just prior to both contact lens insertion and removal provides a cushion for the lens, and facilitates removing it, respectively.
INFECTIOUS CONJUNCTIVITIS
Diagnosis. The hallmark sign of bacterial conjunctivitis is a yellow-white mucopurulent discharge, combined with papillae of the palpebral conjunctiva, bulbar conjunctival chemosis, and hyperemia.
The symptoms include discomfort, a foreign-body sensation, and the eyelashes sticking together, especially upon waking.
Viral conjunctivitis presents clinically as conjunctival redness, chemosis, and a watery discharge. There may be palpebral conjunctival follicles, corneal subepithelial infiltrates (SEI), and a palpable preauricular lymph node.
The symptoms include itching, burning, foreign-body sensation, and/or a recent history of respiratory tract infection.
Infectious conjunctivitis stems from exposure to pathogens, whether from the air or from contaminated hands during lens insertion and removal. Humans are notoriously poor at proper handwashing.5 In addition, pathogens can adhere to deposited contact lenses, resulting in infection.
Treatment. Treatment for bacterial conjunctivitis includes topical antibiotics qid for five-to-seven days, with follow-up every two to three days initially, and then every five to seven days until resolved. Because viral conjunctivitis is typically self-limiting, the treatment is palliative. Specifically, it includes cool compresses, artificial tears, and vasoconstrictors. Topical steroids may be added, then tapered later if no herpes simplex infection is detected and if the SEI are not resolving.6
INFECTIOUS KERATITIS
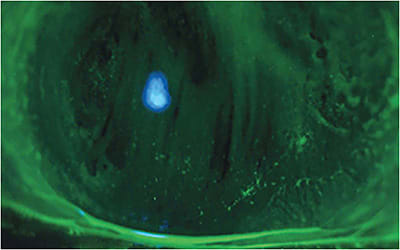
Diagnosis. Acanthamoeba keratitis, highly associated with soft contact lens wear, appears as bulbar conjunctival hyperemia, corneal inflammation, a dendritiform epithelial pattern (often mistaken for herpes simplex keratitis), radial keratoneuritis — linear, branching infiltrates in the mid-stroma along the corneal nerves, and a non-pathognomonic ring infiltrate, making diagnosis initially tough.
The symptoms include severe pain, which is disproportionate to the level of bulbar conjunctival hyperemia. In addition, corneal inflammation is present.
Ulcerative bacterial keratitis presents differently, depending on the organism involved. Typically, the signs include moderate to severe pain, photophobia, decreased vision, and mucopurulent discharge. Upon slit lamp examination, an epithelial defect that stains positively with sodium fluorescein is accompanied by stromal loss and edema; an anterior chamber reaction is also frequent. Common causes include Staphylococcus, Streptococcus, Moraxella, Serratia, and Pseudomonas species. The latter is highly correlated with soft contact lens wear. Experts recommend culturing infiltrates larger than 1 mm to 2 mm, in the visual axis, or if an unusual microorganism is expected. For early cases, this is to confirm the bacterial etiology; for unresponsive ones, to determine the exact organism of etiology such that the most efficacious antibiotic against that organism can be utilized.
Treatment. As 90% of those patients who have Acanthamoeba keratitis are soft contact lens wearers,7 40% are noncompliant with their lens care,8 and 32% wear their lenses while swimming, re-educating patients about the importance of adhering to their care regimen and wearing schedule is paramount. It is recommended that primary eye care providers refer the patient to a corneal specialist, who may prescribe topical polyhexamethyl biguanide, chlorhexidine, propamidine isethionate, an antibiotic, and/or voriconazole or miconazole, all around the clock. Oral ketoconazole or voriconazole can be used as adjunctive therapy, with atropine optional for comfort. There are no anti-amoebic ophthalmic solutions on the market, so the treatment may vary. The condition may take up to a year to completely resolve.9
For bacterial keratitis, treatment depends on the lesion’s severity. Topical antibiotics q1h to q2h, to fortified antibiotics around the clock, to hospital admission for intravenous antibiotics can be prescribed. Infectious keratitis can be sight-threatening if it is not promptly and successfully treated.
MAINTAINING WEAR
Because soft contact lens-induced red eye is bothersome and can potentially cause debilitating loss of vision, it is imperative that ODs accurately identify and treat the cause. Patients enjoy wearing their contact lenses, and desire returning to their lens wear soon and without incident. OM
More on Red Eye
Merchandising Red Eye? bit.ly/OM1302RedEye
Cornea: Contact Lens Complicationsbit.ly/OM1801CLComplications
Insights Into Ocular Rednessbit.ly/OM2202OcularRedness
REFERENCES
- Pucker AD, Tichenor AA. A Review of Contact Lens Dropout. Clin Optom (Auckl). 2020; 12: 85–94. doi: 10.2147/OPTO.S198637.
- Brennan NA, Efron N, Bruce AS, Duldig DI, Russo NJ. Dehydration of hydrogel lenses: environmental influences during normal wear. Am J Optom Physiol Opt. 1988;65(4):277-281.
- Bibby MM. Sagittal depth considerations in the selection of the base curve radius of a soft contact lens. Am J Optom Physiol Opt. 1979;56(7):407-413. doi: 10.1097/00006324-197907000-00001.
- Gromacki S. Contact Lens Spectrum. Soft Contact Lens Deposition- Part 1. https://www.clspectrum.com/issues/2006/february-2006/contact-lens-care . February 1, 2006. Accessed December 6, 2022.
- Gromacki SJ. Hand-Washing: the Consequences. In: Care Solution Corner, Cont Lens Today 2012; April 15:3.
- Millard KA, Groemminger S, Cavet M et al. Time course evaluation of residual hydrogen peroxide and in vitro effects of peroxide lens care solutions. Optom Vis Sci. 2011;E-abstract 115385.
- Bennett ES. Contact Lens Spectrum. Acanthamoeba keratitis in 2007: Stay informed but calm. https://www.clspectrum.com/issues/2007/july-2007/readers-forum July 2007. Accessed December 6, 2022.
- Guttman C. Ophthalmology Times. Acanthamoeba keratitis increasing at alarming rate. https://www.ophthalmologytimes.com/view/acanthamoeba-keratitis-increasing-alarming-rate . Jan. 1, 2006. Accessed December 6, 2022.
- Gromacki SJ and Johnson D. Acanthamoeba Keratitis: A Patient’s Perspective. Review of Cornea and Contact Lenses 2008;145(8):18-21.




