Vision typically changes dramatically with pupil size variation, and for some there is great difficulty in perceiving anything in clear focus because they have large amounts of higher-order aberrations.
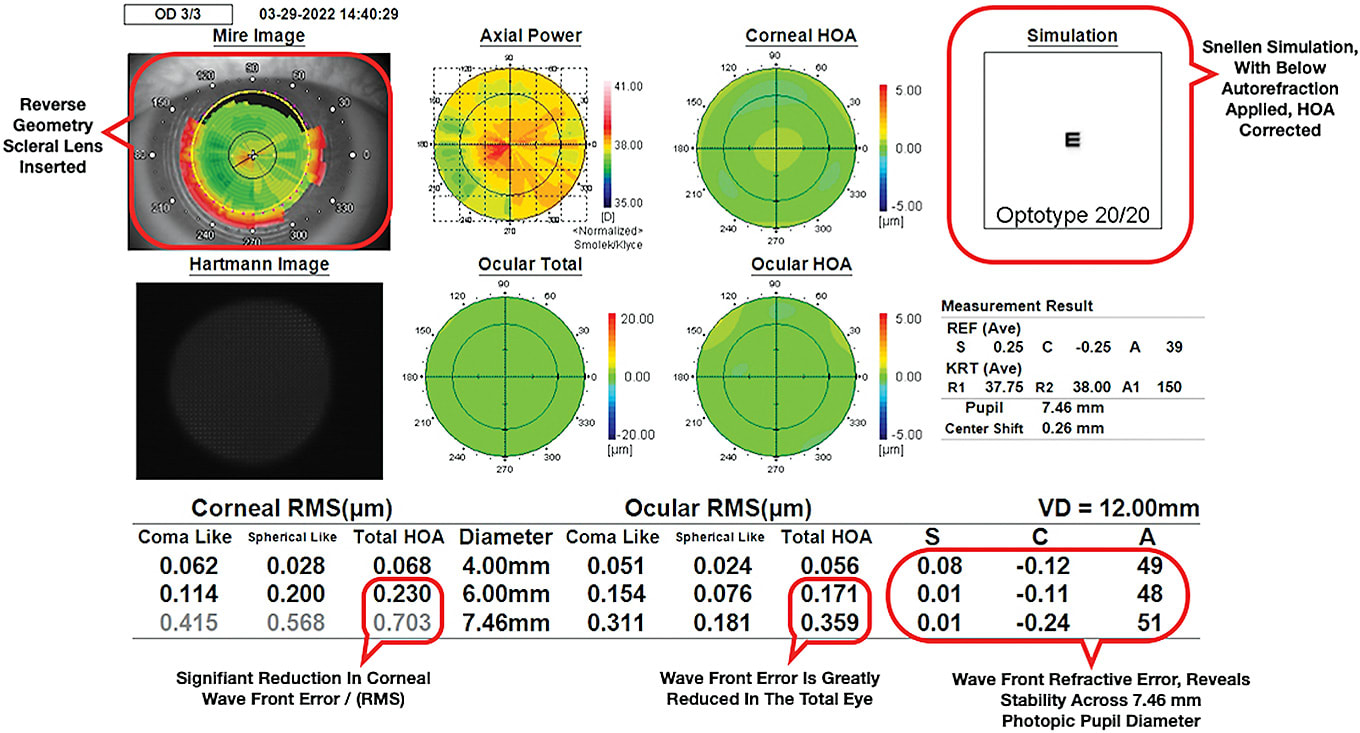
Scleral contact lenses, assisted with data taken from aberrometry, often help reduce the higher and lower-order aberrations of my practice’s patients by 50%. Scleral lenses also have solved obvious problems for our patients, such as keratoconus, as well as some not so obvious problems, such as photophobia and migraines headaches.
Here, I discuss the process for conducting wavefront aberrometry for scleral lens selection, to help patients achieve clearer and more comfortable vision.
STEP ONE: INITIAL EXAMS & SETTING EXPECTATIONS
Every exam that I perform in our clinic begins with the patient reviewing a snellen simulation of a 20/20 letter, for both their right eye and left eye. There are times when the simulation is very focused, and times when the snellen letter is not legible at all.
During these initial exams, it’s important to listen to patients and set proper expectations for them. Patients want doctors to understand that images are not just out of focus, they may also have halos, starbursts, or glares, to name a few. When we demonstrate how our instruments can calculate visual distortion, it helps patients know we understand their vision problems.
Failing to set proper optical expectations, especially when our patients are already visually frustrated, almost always results in glasses remakes, or multiple contact lens trials. Knowing when we are not going to be able to deliver a clear focus to one or both eyes saves time and frustration for both the doctor and the patient.
Stability in refractive error is reviewed with our patients, if needed. Patients with large changes in sphere, cylinder, and axis at different pupil sizes can be helped significantly with scleral lenses by using larger optical zones and in many cases reverse geometry designs.
The patient’s pupil size in photopic conditions is reviewed, and if there are complaints about night vision, pupillometry is performed in addition to conducting basic topography, keratometry, aberrometry, auto-refraction, and photopic pupil size acquisition as needed.
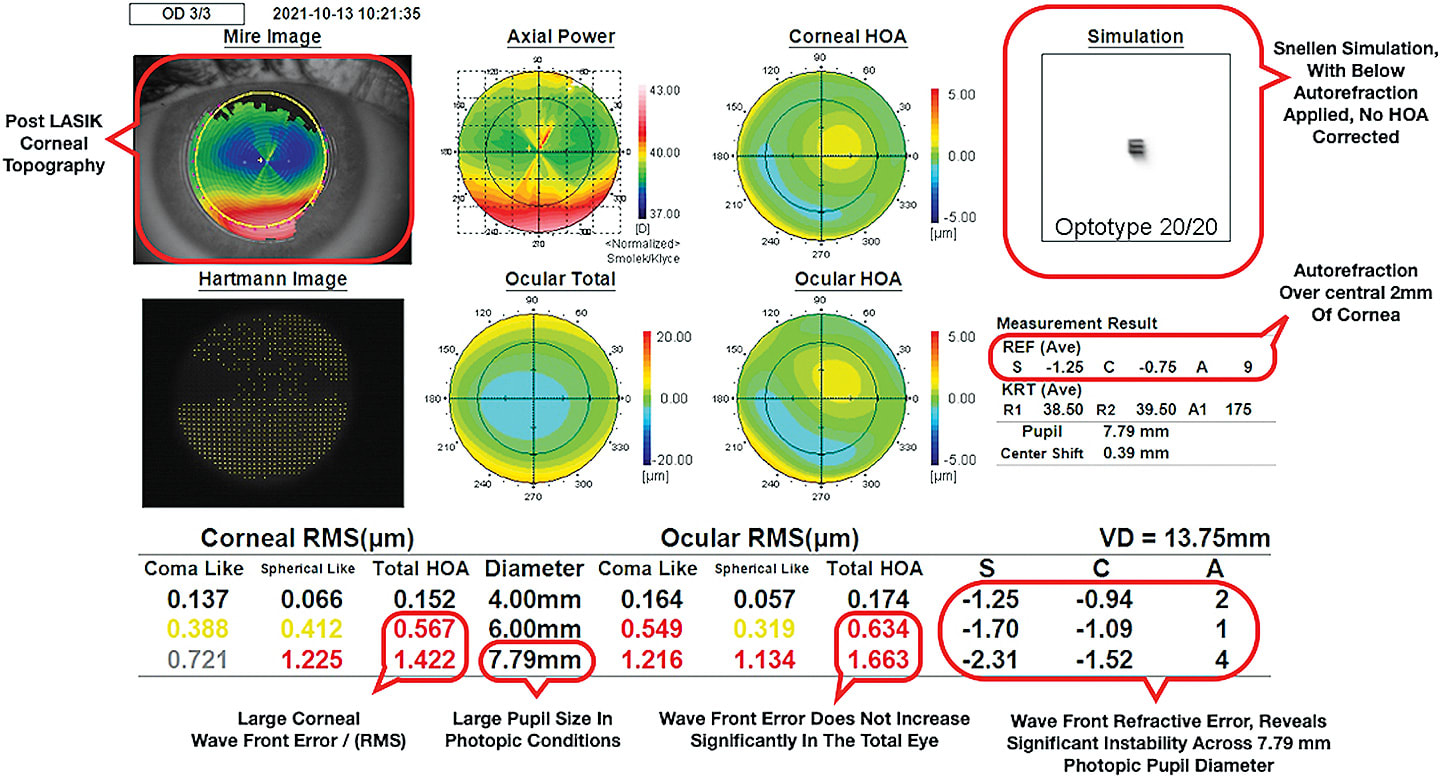
This is a good time to be reminded that auto-refraction, at best, provides information based on the central 2 mm visual pathway. Aberrometry considers whatever surface area is relevant, from full light, normal light, and at largest scotopic vision pupil size. We have found scotopic aberrometry to be very helpful in revealing the full extent to which night vision may be compromised by changing lower-order and higher-order aberrations.
STEP TWO: MEASURING RMS
Once aberrometry data is obtained, the aberrometer can evaluate the root mean square, or RMS, which effectively quantifies the size of the wavefront aberration. RMS values are reviewed at small and large pupil size. Aberrations with RMS value over 0.30 µm can be considered clinically significant if pupils are less than 4 mm in regular daytime lighting.
Patient Case: The Comic Book Illustrator
A scleral lens patient, a 35-year old comic book illustrator, recently presented complaining that glasses and daily disposable contact lenses were not providing clear vision, especially at far distances.
The patient reported tolerable night vision, but car headlights caused significant starbursts; additionally, the patient said their eyes felt dry, with or without contact lenses, and they were unsure about continuing with soft contact lenses.
A separate pair of glasses were required for their 10+ hours a day of computer-aided comic illustration.
CLINICAL FINDINGS
The patient’s best-corrected VA with spectacles was OD 20/30 and OS 20/25, with noticeable ghosting and shadowing upon reading snellen letters. The patient was unable to tolerate higher levels of myopia or cylindrical correction in the phoropter because of visual discomfort and confusion.
Examination revealed no family history of ocular disease, and spectacle prescription changes were minor. Ocular surface evaluation revealed low-grade diffuse superficial punctate keratitis OU.
The patient was encouraged to take frequent breaks from their computer, to relax their focusing, and to be deliberate with blink exercises. The patient was encouraged to return to our clinic for scleral profilometer mapping, and for a scleral lens fitting. Soft contact lens wear was discontinued, and a regimen of rewetting drops was prescribed for use four to six times per day.
FOLLOW-UP
After completing the scleral lens fitting process, our patient was able to see OD 20/20+2, and OS 20/20-1. Separate corrections were no longer needed for computer work, and the patient’s vision felt more relaxed and focused at both distance and near.
After two weeks of wear, the patient’s comfort and dryness have improved and their wearing time has gradually increased to 10 to 12 hours per day. The patient’s starbursts from car headlights have been eliminated.
Aberrometry revealed a significant reduction in the patient’s higher-order aberrations, with minimal shift in first-order refractive error from 4mm to 6mm pupil changes. Simulated snellen acuity significantly improved.
For those patients who have visually demanding careers, combined with complex visual challenges, aberrometry can often help set a proper course for best visual outcome.
RMS values approximately double for every 1 mm increase in pupil size. Larger pupils (more than 6 mm in normal lighting or photopic conditions) can tolerate larger aberrations, as distortion is spread over a larger surface area and is often less bothersome.
RMS values exceeding 0.40 µm should be considered as having significant visual impact even for pupils over 4 mm in diameter.
STEP THREE: ANALYZING THE DATA
The source of the aberrations is reviewed to determine the practicality of correcting them with scleral contact lenses, as some aberrations are too complex to be corrected with standard scleral lens designs.
The most common separation of aberrations will be corneal and internal. Corneal aberrations may be separated further by tear film, anterior, and posterior corneal surface.
Based on my own experience at my practice, most aberrations of the tear film and anterior corneal surface are greatly reduced while the patient is wearing scleral lenses. Up until the most recent scleral lens designs, I found posterior corneal surface and other internal aberrations were often impossible to correct.
The more obvious problems are looked for, including K readings over 46 for early keratoconus consideration, irregular astigmatism, corneal deformities, post-LASIK, radial keratotomy, corneal transplant, and of course, moderate or severe keratoconus.
SEEING MORE CLEARLY
Aberrometry is the heart of our practice, and challenges our understanding of our patients’ optical perception of the world around them. Our clinics have experienced tremendous growth since the addition of aberrometry.
For my patients who have found success with scleral lenses, they now feel safer when driving as they are now able to see consistently across a variety of lighting conditions. Relaxed vision takes on a whole new meaning, as glare is reduced, overcorrection eliminated, and aniseikonia a thing of the past.
Our patients need our help, and with the proper understanding and use of aberrometry we can find more patients who can benefit from scleral contact lenses. Scleral lenses can provide clear, protected, and relaxed vision. OM




