At our clinics, we always educate our patients that treating dry eye disease (DED) is a marathon, and not a sprint. It is common for patients to have at-home therapies or “homework” they need in order to manage their DED. When the patient comes to your practice for an office visit, you can use in-office treatments that complement their at-home care. This article will help determine the best way to complement treatment for each patient, based on the type of DED they have.
Aqueous deficient dry eye
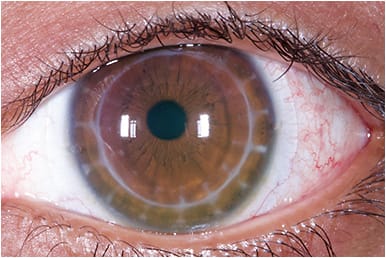
Addressing aqueous deficient dry eye can be challenging. One at-home therapy option, which is also convenient for contact lens wearers since it is not in an eye drop form, is a dry eye relief nasal spray. This nasal spray helps aqueous deficient dry eye by increasing tear production. You may also prescribe scleral contact lenses (Figure 1) for your patient for at-home care, which can be used as part of a holistic treatment1 and have become increasingly common as a treatment for ocular surface disease.2 Scleral lenses protect the cornea, accelerate the healing process, and decrease the frequency of topical lubricants.3
When you see these patients in your practice, you can complement their treatment by prescribing immunomodulators, autologous serum drops, or punctal plugs. These may be used in combination with a nasal spray or scleral lens option.
It is also helpful to remind all patients to take frequent breaks on digital devices and utilize the 20-20-20 rule: every 20 minutes, look at something 20 feet away for 20 seconds.
Artificial tears are also appropriate to use for an at-home treatment as they can be used as a replacement for the eye’s natural tears. It is important to recommend, or prescribe, a specific type of artificial tear, since various types of artificial tears have preservatives that are toxic to the ocular surface.
Blepharitis
Good at-home eyelid hygiene, such as eyelid scrubs, foam wipes, and hypochlorous acid sprays to maintain tear film integrity, is imperative for treating blepharitis. Applying a warm compress to the meibomian glands to improve secretion4 can also be an effective treatment.
As blepharitis is commonly caused by excess Demodex (Figure 2), we educate our patients on how to perform their daily home therapy when they visit the clinic. Sometimes, a patient’s blepharitis can become so problematic that it is difficult to manage at home. In these cases, in-office devices that can clean the lids and lashes more thoroughly should be used. These can clean the lids and lashes better than home therapy alone, similar to going to the dentist for a professional teeth cleaning.

Meibomian gland dysfunction
This evaporative type of dry eye occurs in over 85% of DED patients.5 In these types of patients, warm compresses and lid massages can be helpful at-home treatments to keep the meibomian glands from becoming obstructed. Our practices also recommend using commercial heated eye masks for 10 minutes, at times followed by massage, twice per day, as well as daily lid hygiene.
When seeing these patients in clinic, if these at-home treatments are not enough, their excess meibum can be melted using meibomian heating devices. Their glands can then be expressed by either a pulsation device or by hand. Additionally, intense pulsed light (IPL) therapy can treat MGD (Figure 3). Ocular rosacea (see below) and MGD often occur concurrently, causing DED symptoms. Therefore, IPL helps to treat the root cause of dry eye. Please note that the heat from warm compresses can sometimes exacerbate the redness in lids of patients with ocular rosacea. If that is the case, warm compresses may not be recommended for these patients.

Ocular rosacea
As there is a strong association between a high concentration of Demodex and ocular rosacea,6 similar daily lid hygiene routines can be followed for home therapy. Ocular rosacea can also be triggered by lifestyle factors such as overexposure to the sun, which is why SPF 30 or higher sunblock is recommended.
In our clinics, if ocular rosacea is a main contributing factor to the patient’s dry eye, an excellent in-office treatment option is IPL therapy. IPL works by using bursts of light at specific wavelengths to target the abnormal blood vessels, called telangiectasias, that occur in patients with ocular rosacea (Figure 4). These abnormal blood vessels on the lid margin can release pro-inflammatory mediators, thus contributing to ocular surface disease. In our office, we do four IPL treatments, spaced 3-4 weeks apart.

When a patient is undergoing IPL treatment, they should still continue their lid hygiene practices at home. In addition, it is important to wash their face with a gentle cleanser and avoid any harsh ingredients such as glycolic acid. It is important that patients continue to protect themselves from excess sun exposure and use sunblock with SPF 30 or higher while receiving IPL treatments.
Working hand-in-hand
In-office therapies and at-home therapies work hand in hand to treat and manage a variety of causative factors that contribute to the signs and symptoms of DED. Educating our patients on both types of treatment modalities and how they can work synergistically is an important part of our patients’ continued success. OM
REFERENCES
- Thulasi P, Djalilian A. Update in Current Diagnostics and Therapeutics of Dry Eye Disease. Ophthalmology. 2017;124:S27–33.
- Bavinger JC, DeLoss K, Mian SI. Scleral lens use in dry eye syndrome. Curr Opinion Ophthalmol. 2015 Jul;26(4):319-24.31.
- Stoyanova EL, Otten HM, Wisse R, et al. Bandage and scleral contact lenses for ocular graft-versus-host disease after allogeneic haematopoietic stem cell transplantation. Acta Ophthalmol. 2015 Nov;93(7):e604.
- Geerling G, Tauber J, Baudouin C, Goto E, Matsumoto Y, O’Brien T, et al. The International Workshop on Meibomian Gland Dysfunction: report of the subcommittee on management and treatment of meibomian gland dysfunction. Invest Ophthalmol Vis Sci. 2011;52(4):2050-2064. doi:https://doi.org/10.1167/iovs.10-6997g .
- Findlay Q, Reid K. Dry eye disease: when to treat and when to refer. Aust Prescr. 2018;41:160-163.
- Gonzalez-Hinojosa D, Jaime-Villalonga A, Aguilar-Montes G, Lammoglia-Ordiales L. Demodex and rosacea: Is there a relationship? Indian J Ophthalmol. 2018;66:36-38.





