Testing for dry eye disease (DED) is important for several reasons:
- Patients expect their optometrist, as their primary eye care provider, to identify DED, among other ocular conditions.
- The condition’s symptoms, such as burning, itching, and foreign body sensation, can have a negative effect on a patient’s quality of life.
- DED can induce intermittent blurry or fluctuating vision, leading to an inaccurate prescription.
- DED can cause incorrect biometry readings, resulting in IOLs that contain the wrong prescription. (Incidentally, many ophthalmologists are making the DED diagnosis preoperatively.)
- DED can lead to permanent vision loss if left untreated.
- DED can prevent successful contact lens wear and prompt contact lens dropout.
- A familiarity with the testing options available may be advantageous in confirming the optimal DED treatment plan for your patient.
In addition to the tried and true DED diagnostic measures, such as corneal staining and tear break up time, here, I discuss the objective tests available to aid in identifying DED and when to use them. This way, ODs can both meet their patients’ eye care expectations and prescribe the needed treatment(s). (See “Treat Dry Eye Disease by Severity,” p.22.)
Matrix metalloproteinase-9 testing
Inflammatory markers, including matrix metalloproteinase-9 (MMP-9), are elevated in the tear film of DED patients.1,2,3 Specifically, studies suggest that MMP-9 production increases in response to the hyperosmolar condition of the tears in DED patients.1,2,3 Additionally, positive MMP-9 results have been associated with shorter tear break-up time (TBUT less than 3 seconds), and higher corneal staining scores.2 Further, measuring MMP-9 in the tear film can help to identify ocular surface inflammation, and has been shown to correlate with DED symptoms and signs.1,2,3
MMP-9 diagnostic testing tools provide qualitative (yes/no) results with a sensitivity of 81% to 85% and a specificity of 94% to 98%.2,3 That said, it is important to be mindful of potential false positives that may occur due to an error in sample size, or if a patient is already being treated with a medication that inhibits metalloproteinase activity.
When to use. Several studies show a strong connection between increased MMP-9 levels in the tear film of patients who have a wide variety of ocular surface conditions, including: Sjögren’s syndrome, meibomian gland dysfunction (MGD), keratoconus, vernal keratoconjunctivitis, conjunctivochalasis, and extended contact lens wear.4
Tear osmolarity testing
Normal tear osmolarity ranges from 275 mOsm/L and 307 mOsm/L, with greater than 308 mOms/L or a difference of 8 mOsm/L between each eye, requiring further investigation.5 When tear volume is reduced, the osmolarity of the tears increase.5 Whether caused by an increased evaporation rate or a reduction of tear secretion, this hyperosmolarity of the tears is indicative of reduced aqueous layers.5
Hyperosmolarity can affect the corneal nerves, causing distressed epithelial cells to worsen the inflammatory cascade. This increases levels of pro-inflammatory mediators, such as MMP-9, cytokines, and proteolytic enzymes,4,5 which causes burning and stinging. In chronic cases, hyperosmolarity can lead to further loss of goblet cells, decreased mucin production and tear film instability, and possibly even cell death, which may also contribute to neurotrophic inflammation.4,5
When to use. Tear osmolarity testing should be used to determine DED severity.
Blink rate tests
Abnormal blinking may result in poor tear film distribution and excessive exposure of the ocular surface.6 A decreased blink rate and an increased number of incomplete blinks have been associated with digital device use.6
It can be confusing for a patient who has DED symptoms to understand why their lack of blinking is correlated with having to blink frequently to clear an image (in an attempt to compensate for the acquired tear film instability).6 Filming a patient’s blink pattern, so they can witness the partial or incomplete blinking themselves can sometimes be a helpful tactic to get them to understand that a full blink is necessary for tear film homeostasis.
When to use. A decreased blink rate has been associated with screen use,7 botulinum toxin injections,8 and in patients who have neurological conditions, such as Parkinson’s disease.9 Clinically, it is easy (and free) to monitor blink rate if you have a slit lamp; therefore, I like to assess blink rate on all patients, especially on symptomatic patients.
Meibography
Determining the health of the meibomian glands and eyelid function via photo documentation aids in the diagnosis and monitoring, as well as patient education of DED. This is because the meibomian glands secrete lipids that help support tear production.10,11 Optical coherence tomography, meiboscopy, laser confocal microscopy, and at-the-slit-lamp mobile phone camera technology are the options available for meibography.
When to use. In a perfect world, there would be baseline meibomian gland imaging on all patients. It is non-invasive, easy to obtain, and beneficial to document and monitor for changes over time, even in “healthy” and “asymptomatic” patients. Unfortunately, there is a very long list of things known to affect MG function, including: age, rosacea, history of atopy, psoriasis, androgen deficiency, and Sjögren’s syndrome to name a few.12,13
In addition, other factors, like tattoo eyeliner, contact lens wear, Demodex folliculorum, and chronic blepharitis predispose a patient to MGD.12
Also, certain medications, such as isotretinoin for acne, hormone replacement therapy, antidepressants, and systemic use of antibiotics may all have an effect on MG.12

Tear volume
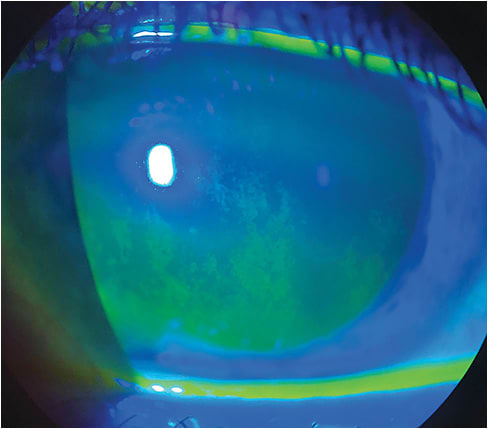
Because aqueous tear deficiency is characterized by inadequate tear production, the measurement of tear volume can assist in the DED diagnosis, as well as establish a baseline before treatment. Tear volume can be determined via Schirmer’s test, strip meniscometry, tear meniscus height, and fluorescein TBUT.
When to use. Tear volume can be helpful to know when establishing a baseline before treatment. Aqueous tear deficiency is characterized by inadequate tear production with predominant causes, including Sjögren’s syndrome, lacrimal gland dysfunction, and/or systemic drugs (i.e. antihistamines, decongestants diuretics, beta-blockers).14 An assessment of the tear meniscus may help provide the clues that additional therapies, such as punctal plugs, nasal neurostimulation, and/or autologous serum tears, may be needed to increase tear volume.14 Although easy to test, repeatability of measuring tear volume may be poor, so more research is needed in this area.
Accuracy
With the availability of these testing tools, ODs can determine the specific cause of DED and, thus, prescribe the most appropriate treatment. This, in turn, provides the DED patient with symptomatic relief, reinforcing the OD’s expertise in eye care. OM
References
- Park JY, Kim BG, Kim JS, Hwang JH. Matrix Metalloproteinase 9 Point-of-Care Immunoassay Result Predicts Response to Topical Cyclosporine Treatment in Dry Eye Disease. Transl Vis Sci Technol. 2018;7(5):31. doi: 10.1167/tvst.7.5.31.
- Lee YH, Bang SP, Shim KY, Son MJ, Kim H, Jun JH. Association of tear matrix metalloproteinase 9 immunoassay with signs and symptoms of dry eye disease: A cross-sectional study using qualitative, semiquantitative, and quantitative strategies. PLoS One. 2021;16(10). doi: 10.1371/journal.pone.0258203.
- Lanza NL, Valenzuela F, Perez VL, Galor A. The Matrix Metalloproteinase 9 Point-of-Care Test in Dry Eye. Ocul Surf. 2016;14(2):189–195. doi: 10.1016/j.jtos.2015.10.004.
- Lemp MA, Bron AJ, Baudouin C, et al. Tear osmolarity in the diagnosis and management of dry eye disease. Am J Ophthalmol. 2011;151(5):792–798.e1. doi: 10.1016/j.ajo.2010.10.032.
- Versura P, Profazio V, Campos EC. Performance of tear osmolarity compared to previous diagnostic tests for dry eye diseases. Curr Eye Res. 2010;35(7):553-564. doi: 10.3109/02713683.2010.484557.
- Al-Mohtaseb Z, Schachter S, Shen Lee B, Garlich J, Trattler W. The Relationship Between Dry Eye Disease and Digital Screen Time. Clin Ophthalmol. 2021; 15: 3811–3820. doi: doi: 10.2147/OPTH.S321591.
- Zaina Al-Mohtaseb, 1 Scott Schachter, 2 Bridgitte Shen Lee, et. Al . The Relationship Between Dry Eye Disease and Digital Screen Time. Clin Ophthalmol. 2021; 15: 3811–3820. doi: 10.2147/OPTH.S321591
- Yazdanpanah G, Yen MT, Pflugfelder SC. Quantitative assessment of botulinum toxin injection on blink rate in blepharospasm. Orbit. 2022;1-8. doi:10.1080/01676830.2022.2151628.
- Ortega J, Plaska CR, Gomes BA, Ellmore TM. Spontaneous Eye Blink Rate During the Working Memory Delay Period Predicts Task Accuracy. Front Psychol. 2022;13:788231. doi:10.3389/fpsyg.2022.788231
- Fineide F, Arita R, Utheim TP. The role of meibography in ocular surface diagnostics: A review. Ocul Surf. 2021;19:133-144. doi: 10.1016/j.jtos.2020.05.004.
- Fineide F, Arita R, Utheim TP. The role of meibography in ocular surface diagnostics: A review. Ocul Surf. 2021;19:133-144. doi:10.1016/j.jtos.2020.05.004
- Schaumberg DA, Nichols JJ, Papas EB, Tong L, Uchino M, Nichols KK. The international workshop on meibomian gland dysfunction: report of the subcommittee on the epidemiology of, and associated risk factors for, MGD. Invest Ophthalmol Vis Sci. 2011 Mar;52(4):1994-2005.
- Wang Y, Xu Z, Gong Q, et al. The Role of Different Tear Volume Detection Methods in the Evaluation and Diagnosis of Mild Dry Eye Disease. Transl Vis Sci Technol. 2022;11(3):15. doi:10.1167/tvst.11.3.15
- Pflugfelder SC, Gumus K, Feuerman J, Alex A. Tear Volume-based Diagnostic Classification for Tear Dysfunction. Int Ophthalmol Clin. 2017;57(2):1-12.




