We are fortunate to be in a time when there are more diagnostic tools as well as treatments for our patients who have diabetic eye disease. Tools such as optical coherence tomography (OCT), optical coherence tomography-angiography (OCT-A), fluorescein angiography (FA), and widefield fluorescein angiography have allowed us to detect diabetic eye disease sooner and in ways we never could before. As such, we can detect subtle changes in retinal structure often before the patient presents with symptoms, such as reduced vision.
However, even with these advanced tools, patient stress and anxiety can still get in the way of an effective examination.
Here, I talk about how to best explain to patients how these devices can help, to put them at ease.
WARMING UP THE PATIENT
Before we even start testing, we need to make sure the patient knows the reason for these diagnostics. For example, when first explaining the need for testing, try this:
“Even if your vision is good, that doesn’t mean your eyes are healthy. It’s not uncommon to see patients with 20/20 vision despite having an advanced disease, such as proliferative diabetic retinopathy or severe glaucoma. That’s why it’s important for all patients with diabetes to have yearly exams with a dilation and ancillary testing as indicated.”
I then explain that “Often a patient can have significant damage from their diabetes, but present with normal vision. Therefore, the real goal is to detect changes before they cause damage and vision loss, as it is easier to fix any diabetes-related issues before significant damage occurs, rather than trying to fix it after. It’s similar to preventative maintenance on one’s car: It’s best to have a routine checkup and learn you need new brakes rather than waiting until you get into an accident after your brakes have failed.”
DILATION
Patients hate dilation. It’s a big inconvenience and can be quite bothersome. I explain this to my patients thusly:
“A dilation truly is necessary to fully assess the health of the eyes; it is currently the standard of care to detect signs of diabetic retinopathy.1,2 Only 50% of eyes are correctly classified for the presence and severity of retinopathy through undilated pupils.”3
Widefield photos and other forms of imaging may suffice for screening or serve as an adjunct to your clinical exam, but do not take the place of a dilated retinal exam with slit-lamp and a 90 D or 78 D lens and binocular indirect ophthalmoscopy for peripheral evaluation. Further, newer studies demonstrate that many early signs of diabetic retinopathy are found in the periphery, and not examining the periphery fully can cause an error in grading the true level of diabetic retinopathy, leading to sub-optimal care.4
Studies have also revealed that patients with predominately peripheral lesions — that is, those almost exclusively in the periphery vs. the posterior pole — are at much higher risk of retinopathy than those with only posterior pole hemorrhaging.4 This, again, highlights the importance of dilation with peripheral assessment of the retina.
FLUORESCEIN ANGIOGRAPHY
Fluorescein angiography is a useful tool in detecting diabetes in patients. It can help look for occult neovascularization, or peripheral ischemia that may not be evident on clinical exam. It also might require the most discussion of any of these procedures, as this is the most invasive of those we have discussed.
When explaining the test to a patient, I say:
“We are going to get a test, where dye is injected into your arm and travels to your eye. Then, we will take photos of your eye over the next 10 minutes or so, to evaluate the circulation of your eye and to look for any areas of leakage or swelling. If you’ve had a CAT-Scan with contrast, or an angiogram of the heart, it is very similar.”
If they ask for more clarification, or ask about safety or potential complications, I explain that side effects from the dye are rather rare, though transient, with nausea, vomiting, and allergic reaction being the most common.5 However, we will obviously be watching for any of these adverse events and can take care of them should any arise. Caution should always take place with patients who have a history of allergies to dyes or severe kidney disease, as the dye is cleared by the kidneys.
FUNDUS PHOTOS
Very few patients have issue with photos due to the photos’ non-invasive nature, although the flash may be annoying to some patients. Fortunately, many of the newer fundus cameras utilize scanning lasers, which reduce flash intensity. If a patient expresses concern about the flash, I explain its effects are only temporary, and in no way are of any harm to the eye.
In my experience, most patients with diabetes have had photos taken in the past, whether in clinic or elsewhere, so there is typically no hesitation about them.
Fundus photos enable the documentation and tracking of changes in the retina and can be a great educational tool for the patient. One script you can follow to explain photography is:
“Fundus photos will allow me to better show you the changes in the retina, and where there are signs of damage. Also, it helps us look for any subtle changes over time, thus ensuring the best possible care. Like the old adage says, ‘a picture is worth a thousand words.’”
Further, wide-field cameras offer views of the peripheral retina. While not a substitute for dilation, you can use these photos in conjunction with your clinical exam to be sure you are not missing even subtle changes.
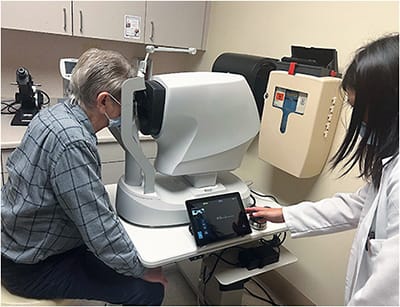
OCT/OCT-A
I like to explain while reviewing or discussing the OCT to patients that we are now fortunate that we have such great testing available to us that has really improved the way we can detect diabetic eye disease. Due to this technology, we can now detect change sooner, and refer for treatment sooner, which should mean better vision for our patients in the long run.
I feel it is prudent to let the patient know we are using the most up-to-date equipment and are doing the most thorough exam possible. It assures the patient they are getting the best exam available, as well as promotes us and our practices as providing superior care with the latest technology.
I have sometimes struggled to explain OCT to patients. Though it’s not entirely accurate, I typically say:
“We are going to take some scans of your eye to further help us look for any diabetic damage.” [If they ask for more information]: “It is similar to an ultrasound, except it uses light waves rather than sound waves to give us a better look inside your eye. We can also use these images following your treatment to show you a ‘before and after’ of how you’ve improved.”
Like fundus photography, most patients do not really feel trepidations about an OCT, as it is relatively innocuous and non-invasive. The flash for the OCT is much less than that of a camera, so most patients are not really bothered by the flash. If an OCT-A is indicated, it does take a tad longer than a traditional OCT, so it can be somewhat difficult in patients who may have an issue sitting still for a period of time.
CREATING EASE
Patients see us for our skill in eye care, and it is, in turn, our responsibility to assist them and make sure they are at ease in our practice, which includes explaining the these tests and any potential deleterious effects.
Only through a collaborative effort with the patient and provider, including appropriate patient education, can we achieve the goal of the best care possible for our patients with diabetes. OM
REFERENCES
- Diabetic Retinopathy Preferred Practice Guidelines. American Academy of Ophthalmology. https://www.aao.org/education/preferred-practice-pattern/diabetic-retinopathy-ppp . Published Oct. 2019. Accessed Feb. 14, 2023.
- American Optometric Association. Diagnosis of Ocular Complications of Diabetes Mellitus. In: Eye Care of the Patient with Diabetes Mellitus. 2nd ed. American Optometric Association; 2019: P. 47.
- Klein R, Klein BE, Neider MW, Hubbard LD, Meuer SM, Brothers RJ. Diabetic retinopathy as detected using ophthalmoscopy, a nonmydriatic camera and a standard fundus camera. Ophthalmology. 1985;92:485-491.
- Silva PS, et al. Peripheral Lesions identified on Ultrawide Field Imaging Predict Increased Risk of Diabetic Retinopathy Progression over 4 Years. Ophthalmology. 2015: 122; 949-56.
- Yannuzzi LA, Rohrer, MA, Tindel LJ, et al. Fluorescein angiography complication survey. Ophthalmology. 1986:93:611-617.




