A total of 2.9 million Americans have low vision (<20/40), and an estimated 5 million Americans will have low vision by 2030, according to the National Eye Institute.1 (See “Low Vision: An Overview,” p.36.) Also, age-related macular degeneration, diabetic retinopathy, and glaucoma have led to more than 19 million cases of moderate or worse vision in adults ages 50 years and older in 2020.2 What’s more, the most common complaint of individuals who have low vision is difficulty reading at near.3 Given these facts, it makes sense for the primary care optometrist to provide, at minimum, basic magnification solutions to these patients.
This article discusses the basic types of magnification options for near viewing: optical magnification tools and electronic video magnification systems. It also briefly mentions other magnification tools. (See “Mainstream Technologies Used for Low Vision,” p.35.)
Optical magnification tools
Optical magnification tools utilize a plus power optical lens, which requires attention to the principles of optics, such as lens size, working distance, and field of view. Some common optical magnification tools:
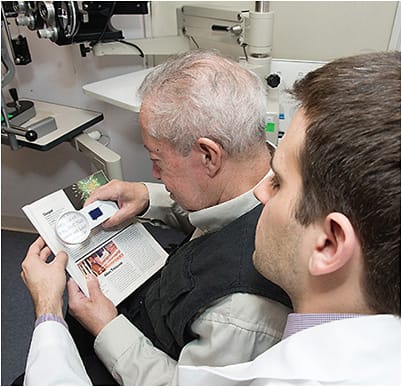
• Handheld magnifiers. Handheld magnifiers are comprised of a plus power lens with a handle. These portable devices may or may not come with an incandescent bulb or LED light. (As a brief reminder, lighting helps with contrast and increased efficiency for near viewing and may lessen the amount of magnification needed. This may be advantageous, as the stronger the magnification power, the lens size and field of view decreases.) Powers range from 3 x to 14 x and are usually printed on the magnifier casing, along with the dioptric (D) value. To use a handheld magnifier, the patient holds it above the reading material at the focal length of the lens power.
Ideal patient candidates. While handheld magnifiers can be used for reading books, among other periodicals, they are ideal for spot reading, given their size and portability. Examples of spot reading items: price tags, receipts, as well as information on products, such as size, amount, and/or nutritional value.
Pro tips for successful use.
- Educate on the power of handheld full-page magnifiers. Many patients will request a magnifier “large enough for an entire page.” Educate these patients that full-page magnifiers give very little power, meaning that while they might provide a large field of view, they do not provide enough magnification.
- Shed a light on the incandescent bulb or LED. Explain to patients that handheld magnifiers that contain an incandescent bulb will eventually need to have their bulb replaced, and that handheld magnifiers that contain an incandescent bulb or an LED will require a battery or charging for continued use. Additionally, show the patient how, specifically, to change the battery.
- Have the patient use their distance correction. Distance correction is used because the lens creates a real image in which light rays emerge parallel. As many patients are used to looking through their bifocal or the reading area of their progressive lens, you will need to educate them that it may take some time to get used to not looking down or tilting their head back. A reading correction can be used with a handheld magnifier. However, the patient must adjust the focal distance of the magnifier closer to the page for clarity of the image.
- Demonstrate focal length. To accomplish this, have the patient hold the magnifier up to a page of text, or object of interest, and pull the handheld magnifier back slowly toward themselves until a clear image appears. Explain that this working distance provides maximum magnification for the patient. For example, a 5 x / 20 D handheld magnifier will have a focal length of →100/20 D = 5 cm. Therefore, the patient will have to hold the magnifier about 2 inches from the material to have a clear image. For this reason, those who cannot maintain the correct position, are unsteady, or have a hand tremor may not be good candidates for a handheld magnifier.
Pro tips for dispensing.
- Create a demo kit. For the primary care practice, we recommend starting with one or two brands that include power ranges from 3 x to 6 x. If there are concerns about stocking, you can always opt for drop shipping or refer to a trusted online resource. Increased powers indicate further functional vision loss, necessitating a referral to a low vision specialist or organization where other advanced devices and programs are available.
- Speak in terms of diopters. There is no uniform standardization for x-notation among different manufacturers. This means a 5 x magnifier might equal 16 D for one brand but equal 20 D in another. As a result, I have found it best to speak to patients in terms of diopters, should they elect to purchase a handheld magnifier outside a primary care practice.
- Make certain patients are using the proper correction and to increase the field of view, instruct the patient to bring themselves closer to the magnifier.
• Stand magnifiers. Stand magnifiers can be made up of a handle with or without a light (incandescent or LED), which inserts into a plastic-encased optical lens with support or is just the lens itself, known as a dome-shaped magnifier. Their size and weight make them less portable. Additionally, as is the case with handheld magnifiers, they come in powers ranging from 3 x/~8 D to 14 x/~56 D. Dome-shaped magnifiers usually come in powers below 12 D. Further, their working distance is set, yet short, providing a virtual image that results in divergent emerging rays of light. This requires a near prescription, or the patient looking through their near bifocal or progressive.
Ideal patient candidate. Stand magnifiers have support or legs that rest on the page, making them steady and easy to use for someone who is unsteady or has a hand tremor. Additionally, patients who have less than a +4.00 D add are the best suited candidates for using stand magnifiers. This is due to the fact that the image produced by a stand magnifier lies beneath the surface of the paper being read with a reading add. Reading adds of greater than +4.00 D will place the image above the stand and will blur the image.
Pro tips for successful use.
- Determine the correct amount of magnification needed. You may remember the Kestenbaum Rule from your optometry school days. This can predict the dioptric reading add for reading near print. To determine the amount of reading add needed for a patient to read 20/50 or 1M print size (which is considered newspaper size print), take the inverse of a patient’s best-corrected distance acuity: and then choose the magnifier based on dioptric value:
- 20/200 → Inverse → 200/20 = +10.00 D
- 20/120 → Inverse → 120/20 = +6.00 D
- 20/50 → Inverse → 50/20 = +2.50 D
- Shed a light on the incandescent bulb or LED. As is the case with handheld magnifiers, explain to patients that those stand magnifiers that contain an incandescent bulb will someday need to have their bulb replaced, and that handheld magnifiers that contain an incandescent bulb or an LED will require a battery or charging. Finally, demonstrate for the patient how, specifically, to change or charge the battery.
Pro tips for dispensing.
- Create a simple demo kit that contains one or two dome magnifiers and stand magnifiers from 3 x to 6 x, and speak in terms of diopters.
- Demonstrate proper use by lying the stand magnifier flat on the page for the clearest image and not hovering above the page. Instruct patients to use flat pages, like those found in mail or in newspapers, to read first. Books can be more challenging due to their binders.
- Place the stand magnifier on the page for the patient. Instruct the patient to look into the magnifier, bringing their eye close to the lens. The stronger the stand magnifier, the closer their eye will need to get to the lens to reach the widest field of view. Instruct the patient to move the magnifier across the paper as they are reading. A lap desk, clip board or reading stand may be helpful to get the patient close enough to the lens to increase the field of view of the reading material.
Electronic video magnification systems
Electronic video magnification systems, typically known as Closed-Circuit Television systems (CCTV), project magnified near and distance images on a screen or monitor. These systems:
• Desktop CCTVs. These require printed material to be brought to the device. Specifically, printed materials are placed on a moveable tray. A camera above the tray captures an image in real-time and displays it on a large screen. The tray can be shifted in the x or y plane to view different portions of the material. Magnification is performed either via a knob/button or touch screen options. Several contrast options are available, depending on the make and model. However, most come with the ability for negative contrast (white on black background).
Ideal patient candidate. Glaucoma patients, or those who have light sensitivity, benefit from CCTV’s negative contrast. CCTVs allow a range of magnification from 2 x to 60 x. This enables the patient to vary the magnification, according to the materials they want to read. This is especially beneficial for those who have extreme low vision or have the need to view materials of various sizes. In addition, these devices allow for writing as well.
Some CCTV’s can be fitted with dual cameras allowing for students to view a distance white board and write their notes at the same time.
Pro tips for successful use.
- Make certain that the device is on a stable and level surface. Desktop CCTVs are usually at eye level, so patients should position themselves to reduce any neck or back strain.
- Have patients adjust magnification and type of contrast (i.e., black on white, white on black, yellow on black, etc.), according to their needs. A reading add should be given that is appropriate for the distance the device is being used.
- If there is an x-y table, move the table and not the material to navigate the document.
Pro tips for dispensing.
- Provide magnification, contrast, and any other settings or input to the installer who usually provides training as well. Desktop CCTVs are usually set up and dispensed by a distributor of the brand/manufacturer. Usually, they are just placed on a table and plugged in for use.
- Demo a portable or handheld electronic magnifier to determine benefit prior to purchase.
• Portable and handheld CCTVs. While slightly smaller than desktop versions, portable systems are about the size of some older laptop computers. Many have a carry case and include other options, such as optical character recognition, reading line, and different color contrasts similar to desktop CCTVs. Handheld CCTV systems are slightly larger than a smartphone.
Ideal patient candidate. Those patients who benefit from electronic magnification and want to be more mobile. These devices are ideal for students and for those on the job, as well as for use while grocery shopping or spot reading while on the go.
Pro tips for successful use.
- Find out what the patient is using it for; is it only for shopping or is this being used on the job or for school? Portability matters.
- Find the right device that is comfortable for the patient to use. Some have tactile buttons and others have a touch screen. Some patients may do better with physical buttons.
Pro tips for dispensing.
- If you decide to carry these devices, have two demo devices to show and compare; consider working with a local organization or distributor in your area. There are many brands and types of portable CCTV’s. Sometimes there are too many for an office to carry all of them.
- For reading, glide the device over the document. Many of these devices come with a stand to rest on a page, which can be helpful. Most handhelds are really meant for spot reading, so go over practical everyday uses, such as reading cooking directions, or finding an expiration date on a product.
MAINSTREAM TECHNOLOGIES USED FOR LOW VISION
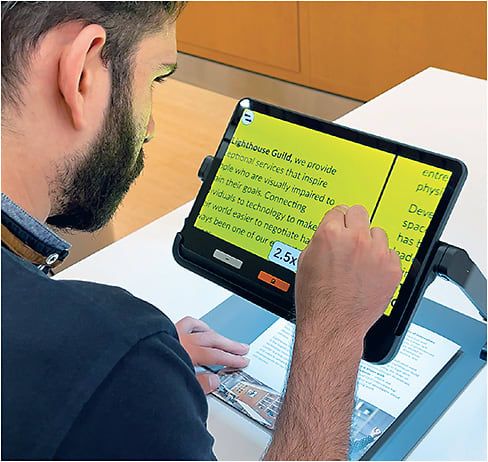
Smartphone and tablet cameras can work as magnifiers, so it’s worth educating the low vision patient about this, if they have not already discovered this on their own.
Additionally, many free magnification apps are available that incorporate the ability to change contrast, brightness, and even artificial intelligence on one’s smartphone and tablet camera.
Simply showing the low vision patient how their smartphone or tablet can be used as a magnifier can make a world of difference to their quality of life. These devices can be used as a magnifier to read a menu, read a sign out loud with optical character recognition, and even describe a scene through artificial intelligence. You can designate a staff member to learn these features and keep up with updates and software changes to maintain ongoing patient education.
Since many patients in the primary care office already have a smartphone or tablet, it may be best to try those magnification options first and compare tasks on follow up with other optical or electronic magnification options.
Interestingly, a study published in 2014 showed that out of 132 people who were blind or visually impaired, two people were told it was possible to use their device by an optometrist.6 As increased awareness and use of these devices have risen since then, it would be interesting to see whether the numbers have improved.
Other tools
Other forms of magnification for reading include bioptics with reading caps, telemicroscopes, and wearable electronic magnification devices.
There are many devices and technologies to choose from. To maximize success, it is important to know which one is right for your patient. Being able to start providing early solutions with basic magnification at your office can help introduce the patient to vision rehabilitation, low vision, and add to their continued independence for the future.
LOW VISION: AN OVERVIEW
Low vision is uncorrectable vision loss that interferes with daily activities. It is better defined in terms of function, rather than [numerical] test results.4 In other words, low vision is “not enough vision to do whatever it is you need to do,” which can vary from person to person.
This functional loss of vision is not correctable by regular glasses, contact lenses, medication, or surgery. Therefore, low vision should not be thought of as having a certain amount or benchmark loss of acuity.
The challenges of low vision may include difficulties with near reading, watching television, shopping, using a computer or smartphone, and driving. Lack of these activities can cause decreased quality of life, loss of independence, and behavioral health issues, such as depression.5
To learn more about low vision services, check out the following resources:
American Academy of Ophthalmology Low Vision Patient Handout. Low Vision - American Academy of Ophthalmology (aao.org )
American Optometric Association. Low Vision (aoa.org )
Council of State Administrators of Vocational Rehabilitation. www.csavr.org/stateagencydirectory
Lighthouse Guild. https://lighthouseguild.org/training/elearning-for-professionals/programs-for-optometrists/
Shuldiner Low Vision Training Institute. Shuldinerlowvisiontraininginstitute.org
The Vision Council. https://whatislowvision.org/find-a-low-vision/
Continuous care
The primary care optometrist is well positioned to provide, at minimum, basic magnification needs early on in someone’s journey with vision loss.
Additionally, they are well positioned to refer patients whose needs exceed this service to a low vision specialist or organizations for more advanced tools, such as low vision spectacles, telescopes, telescopic systems, and head-worn electronic magnification devices, as well as vision rehabilitation programs.
In our experience, most patients who have low vision have never heard of low vision services, nor do they know the field of low vision, let alone any practitioners who work in that area exist. Just educating these patients of these services and professionals makes a huge difference to them.
We recommend having prepared education materials or a folder of resources available for the low vision patient and their family. This should include any local organizations, programs and support, low vision practitioners in your area, and your state’s vision rehabilitation agency. OM
References
- National Eye Institute. Eye Disease Statistics. https://www.nei.nih.gov/sites/default/files/2019-04/NEI_Eye_Disease_Statistics_Factsheet_2014_V10.pdf . Accessed Sept. 11, 2023.
- GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2021 Feb;9(2):e144-e160. doi: 10.1016/S2214-109X(20)30489-7.
- Brown JC, Goldstein JE, Chan TL, Massof R, Ramulu P; Low Vision Research Network Study Group. Characterizing functional complaints in patients seeking outpatient low-vision services in the United States. Ophthalmology. 2014;121(8):1655-62. doi: 10.1016/j.ophtha.2014.02.030.
- American Foundation for the Blind. Low Vision and Legal Blindness Terms and Descriptions. https://www.afb.org/blindness-and-low-vision/eye-conditions/low-vision-and-legal-blindness-terms-and-descriptions#AFunctionalDefintion_of_LowVision . Accessed Sept. 11, 2023.
- Zhang X, Bullard KM, Cotch MF, et al. Association between depression and functional vision loss in persons 20 years of age or older in the United States, NHANES 2005-2008. JAMA Ophthalmol. 2013;131(5):573-81. doi: 10.1001/jamaophthalmol.2013.2597.
- Crossland MD, Silva RS, Macedo AF. Smartphone, tablet computer and e-reader use by people with vision impairment. Ophthalmic Physiol Opt. 2014;34(5):552-7. doi: 10.1111/opo.12136.





