Education can be the key to preventing dry eye disease (DED). Therefore, in this article, I discuss the specific patient education ODs can provide to their patients to help prevent this condition.

“Understand the disease”
Because DED is chronic and progressive, in addition to identifying and managing the condition properly, we should educate all our patients on how to prevent its onset in the first place. When DED is present, it can take many months or longer to fix or improve the damage to the ocular surface that has already been done. As Benjamin Franklin once said, “an ounce of prevention is worth a pound of cure.”
First, because patients don’t always know the symptoms of DED, it is a good idea to educate them about these symptoms. Specifically, we should explain to our patients that DED and ocular surface disease can have a variety of symptoms; including a burning, sandy, gritty sensation in the eyes, redness, itching, fluctuations in vision, visual strain and fatigue and tearing/watery eyes.
“Eat right”
Many patients are unaware that systemic health is directly related to ocular health. In the case of DED, we should inform all our patients that a poor diet can lead to ocular surface disease.1 Specifically, deficiencies in vitamin A, vitamin D, vitamin B12, vitamin C, and malabsorption can cause DED.1
Omega 3 and GLA from Omega 6 fatty acids are known to help improve the signs and symptoms of DED.
When discussing with a patient how to keep the eyes healthy, I ask them about their diet, specifically if they are consuming foods that contain these vitamins and other antioxidants. Additionally, I emphasize the importance of eating fruits, green, leafy vegetables, healthy fats from foods like fish, avocado and nuts, as well as staying well-hydrated. In our clinic we provide a handout, reminding patients about these important nutrients and listing suggestions of foods that are rich in these building blocks. If a patient does not get enough of the “good stuff” from their diet, I suggest they take a high-quality supplement. We give specific ocular nutritional supplement brand recommendations to ensure our patients are getting the right therapeutic dose and formulation.
“Get proper sleep”
It’s no secret that getting good, quality sleep helps our bodies function properly. A recent finding, however, is that poor sleep is connected with the onset of DED.2,3
One study shows sleep disorder (i.e., reduced sleep time, circadian rhythm disturbances, sleep breathing disturbances, etc.) is linked to both the occurrence and severity of DED, and that various risk factors, such as sleep apnea and depression, associated with sleep disorder, are also connected to DED.2
Another study shows that those who have DED have poorer sleep quality, take longer to fall asleep and have a higher risk of unhealthy sleep duration, including deficient sleep or extreme sleepiness, compared with individuals who don’t have DED.3
As an example, it has been shown that sleep deprivation can cause tear osmolarity levels to increase, decreased tear break-up time, and reduced tear secretions, all of which can cause the development and worsening of DED.2,4
Given the connection between poor sleep and the development of DED, it is essential we inquire with patients about their quality/duration of sleep, as well as discuss with them the importance of getting good, quality sleep, so they can prevent DED. This is a discussion that you can have with your patients during their exam or simply have it as a question on their patient history intake form. If a patient divulges an issue with their sleep, we should refer that patient to a sleep specialist for evaluation.
“Follow the 20-20-20 rule”
We know that studies show the extended use of digital devices can cause DED.5,6 We should communicate this to our patients by explaining that digital device use decreases one’s blink rate. Normally, humans blink about 15 times per minute, which refreshes the tear film and keeps the eyes moist.7 But when using a digital device, such as a smartphone or computer, blink rate decreases to 5 to 7 times per minute, creating ocular dryness.7
What’s more, we should educate our patients about the 20-20-20 rule. As a refresher, this rule is to look 20 feet away, for 20 seconds, every 20 minutes during digital device use, to give the eyes the opportunity to blink naturally to refresh the tear film. To help patients remember this rule, I recommend they place a Post-It Note on their computer or set an alarm on their smartphone. If this routine seems too rigid, another option is to simply encourage patients to take regular breaks when doing near work. I suggest patients get up and move their body for 10 minutes every hour when doing near work, if possible, thus promoting physical health also.
“Use eye-friendly tears”
Before seeking a treatment from a doctor for DED symptoms, some patients will reach for something over the counter first. For this reason, I recommend educating all patients, “don’t trust all tears,” as we know some contain preservatives, such as benzalkonium chloride, that can be toxic to the ocular surface and cause DED when used long-term.8
In particular, we should discourage the use of artificial tears that contain the claim that they are “redness relievers.” This is because these drops are often laden with preservatives and other chemicals that can threaten the health of the ocular surface, if used on a continuous basis.
Additionally, we should provide patients with the names of the specific brands of artificial tears that are safe, so they know precisely what to purchase when faced with pharmacy shelves filled with options.
“Practice lid hygiene”
The next critical piece of patient education to prevent the onset of DED is lid hygiene. Patients are often times completely unaware of the importance of cleaning their lids and lashes. They have a skin care routine, a hair care routine, and an oral hygiene routine, but nothing for the daily care of their eye health.
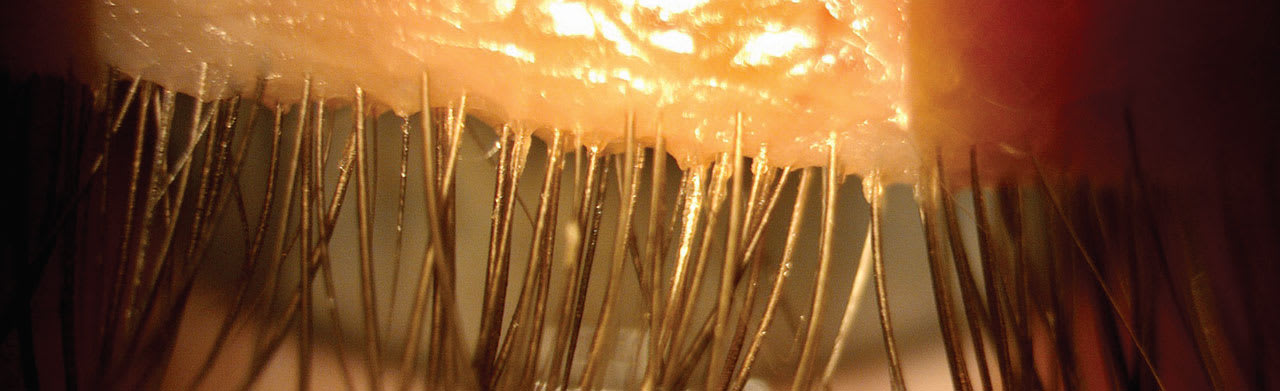
We need to change this by informing them that when their lids and lashes are not clean, they harbor excess bacteria and Demodex mites, which can cause ocular surface disease and DED symptoms.9
Several lid hygiene products are available that are specifically formulated to clean the lids and lashes, and its important it be done on a regular basis. As with artificial tears and ocular nutritional supplements, many different lid hygiene brands are on the market. To prevent confusion, it is important to educate our patients on the specific brand and type of product we want them to use, as well as how they should use it.
“Use ocular cosmetics correctly”
Educating patients on the proper use of ocular cosmetics is another way to prevent DED. The three main points we can educate patients on are:
(1) Removing all eye makeup before going to bed.
(2) Not putting eye liner on the lash margin (i.e., the waterline).
(3) Not using waterproof mascara.
Eye makeup can cause an overgrowth of bacteria and Demodex, which, in turn, can cause dry eye disease. Additionally, placing eyeliner on the lash margin (waterline) can clog the meibomian glands and lead to meibomian gland obstruction and dysfunction, which can cause DED. Something else I’d like you to keep in mind: Waterproof mascara can be difficult to remove, increasing the chances of makeup being left behind even after you attempt to remove it. Patients may have to excessively rub their eyes when attempting to remove waterproof mascara, and this can lead to eye irritation.
“Don’t forget these items!”
In addition to the education discussed above, we should also warn patients about:
• Air conditioner/heater proximity.
• Systemic/allergy medications that can cause ocular dryness.
• Avoiding cigarette use, vaping, and second-hand smoke.
That pound of cure
As illustrated above, there are many areas of patient education we can provide to help prevent the development of DED: eating a healthy diet, getting a good night’s sleep, following the 20-20-20 rule, using the right artificial tear, practicing regular lid hygiene, proper use of eye makeup, and remembering those other important items. It’s worth noting that much of this education can also be used to prevent DED from worsening. I’ve found that patients are more likely to prefer proactive doctors who provide the proper education to maintain excellent eye health. Also, diagnosing and treating DED allows for better care of patients, and provides for more revenue from in-office procedures and sale of products, as well as helps you stand out as an exceptional eye care provider in the community. That “ounce a prevention” can connect to greater practice success! OM
References
1. Serhan HA., Alma’aitah HW, Irshaidat S, Ameer MA, Asghar MS, Tahir MJ. Ophthalmic manifestations of nutritional deficiencies: A mini review. J Family Med Prim Care. 2022; 11(10): 5899–5901. doi: 10.4103/jfmpc.jfmpc_790_22
2. Li A, Zhang X, Guo Y, et al. The Association Between Dry Eye and Sleep Disorders: The Evidence and Possible Mechanisms. Nat Sci Sleep. 2022; 14: 2203–2212. Published online 2022. doi: 10.2147/NSS.S378751.
3. Gu Y, Cao K, Li A., et al. Association between sleep quality and dry eye disease: a literature review and meta-analysis. BMC Ophthalmol. 2024;24(1):152. doi: 10.1186/s12886-024-03416-7.
4. Lee YB, Koh JW, Hyon JY, Wee WR, Kim JJ, Shin YJ. Sleep deprivation reduces tear secretion and impairs the tear film. Invest Ophthalmol Vis Sci. 2014;55(6):3525-31. doi: 10.1167/iovs.14-13881. PMID: 24833736.
5. Golebiowski B, Long J, Harrison K, Lee A, Chidi-Egboka N, Asper L.
Smartphone Use and Effects on Tear Film, Blinking and Binocular Vision.
Curr Eye Res. 2020;45(4):428-434. doi: 10.1080/02713683.2019.1663542.
6. Uwimana A, Ma C, Ma X. Concurrent Rising of Dry Eye and Eye Strain Symptoms Among University Students During the COVID-19 Pandemic Era: A Cross-Sectional Study. Risk Manag Health Policy. 2022:15:2311-2322.doi: 10.2147/RMHP.S388331.
7. American Academy of Ophthalmology. Computers, Digital Devices and Eye Strain. https://www.aao.org/eye-health/tips-prevention/computer-usage. (Accessed May 29, 2024)
8. Baudouin C, Labbe A, Liang H, Pauly A, Brignole-Baudouin F. Preservatives in eyedrops: the good, the bad and the ugly. Prog Retin Eye Res. 2010;29(4):312-34. doi: 10.1016/j.preteyeres.2010.03.001.
9. O’Dell L, Dierker DS, Devries DK, et al. Psychosocial Impact of Demodex Blepharitis. Clin Ophthalmol. 2022:16:2979-2987. doi: 10.2147/OPTH.S374530.




