Blepharitis, a cause of dry eye disease (DED), is most commonly due to Staphylococcus aureus bacteria overgrowth, seborrheic skin conditions, Demodex folliculorum/brevis infestation, or allergic reactions, which can manifest due to exposure to seasonal or environmental allergens, as well as iatrogenic factors. Many medications, such as glaucoma medications, as well as some systemic medications, including biologics used to treat many auto-immune conditions, may cause ocular allergic responses. Lid hygiene tools are essential for both the symptomatic relief and the long-term maintenance of blepharitis, as they effectively manage the issues mentioned. (See “Cutoff Blepharitis from Cosmetics,” below)
Lid hygiene tools fall under two categories: (1) at-home interventions, and (2) in-office interventions:
At-home interventions
The at-home lid hygiene tools:
• Lid cleansers. These contain hypochlorous acid (HOC1), tea tree oil, or okra-derived polysaccharides. HOCl is an antimicrobial most useful in the treatment and maintenance of staph. blepharitis.1 It is applied in spray form to the lids and lashes once to twice daily, and no rubbing or rinsing is needed. Consistency of use is key in controlling staph. bacteria overgrowth.
Many pre-made formulations are sold in spray bottles. While these pre-made HOCl solutions can be difficult for patients to find at retailers, such as in pharmacies and supermarkets, they can be purchased online from the manufacturer or via online retailers in many cases. It is often most advantageous to the patient to be able to purchase them directly from the prescriber’s office. This is how most of my patients choose to buy these solutions. Patients value that I have tested the products we carry in the office for effectiveness and the convenience of being able to purchase them the same day they are prescribed.
Tea tree oil foams contain terpinen-4-ol, which has been found effective in reducing the number of Demodex mites and ocular surface symptoms, such as burning or stinging, associated with Demodex blepharitis.2 It is often recommended for once-to-twice daily use. Consistency is also important here, as recolonization of Demodex is common.
Like HOCl, numerous brands and formulations of tea tree oil foams and gels are widely available at online retailers and often directly from the manufacturers themselves. Regarding tea tree oil formulations, however, extra education and care must be taken to be sure that patients do not confuse our recommended cleansers with natural tea tree oil at full concentration. This is because their use can be damaging to the ocular surface and extremely uncomfortable for the patient. As with most of the products I recommend, I prefer my patients to be able to purchase them directly from my office to avoid confusion and to ensure they are receiving the exact products and formulas recommended.
Okra-based cleansers and products are also available as at-home use cleansers and gel formulas. They can also be used for in-office treatments, often combined with blepharoexfoliation. As with the other lid cleaners, they are available to patients online through the manufacturer, but I recommend in-office sales for the same reasons mentioned above.
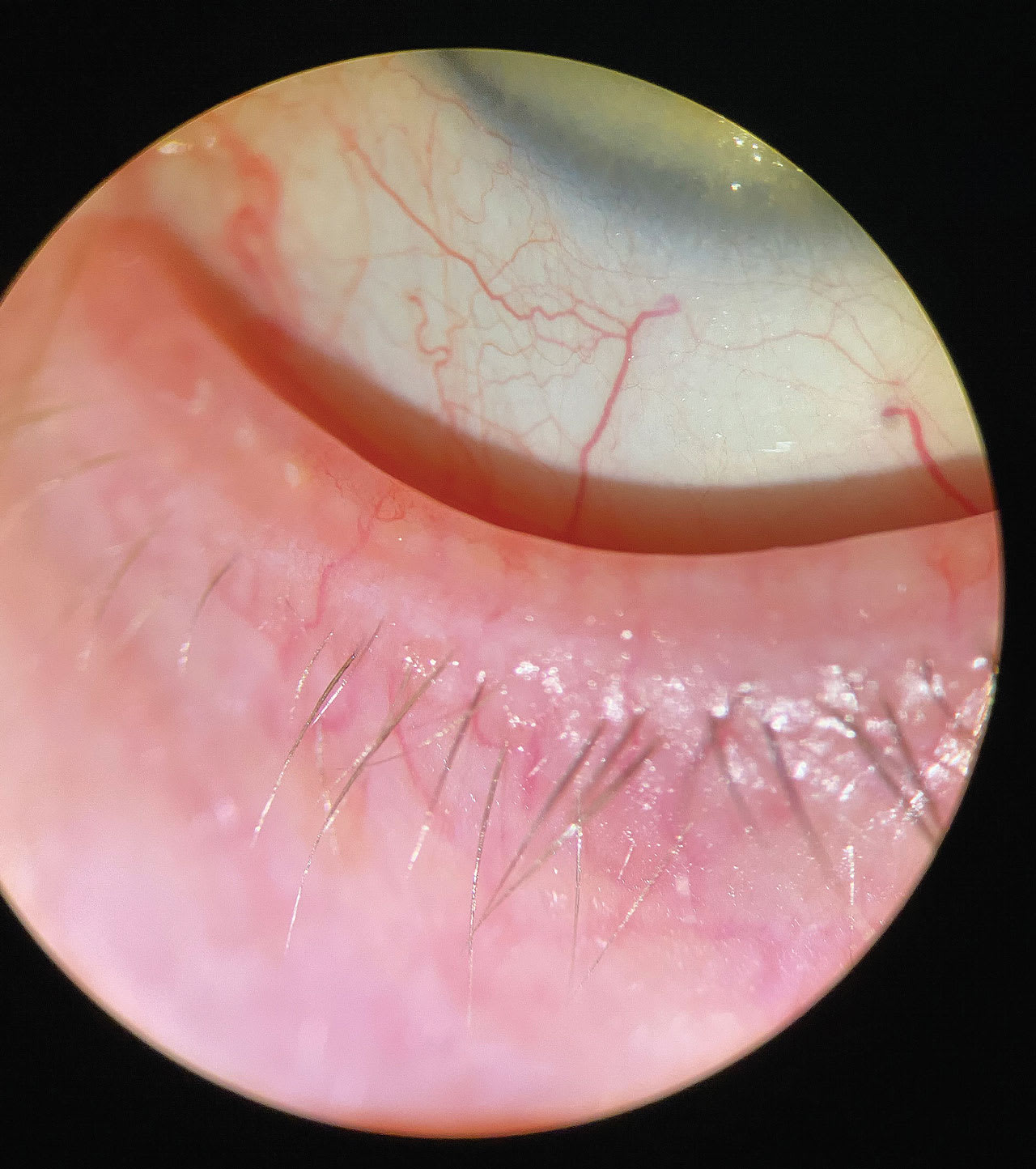
• Topical prescription medication. Topical prescription medication for the treatment of Demodex blepharitis is also an option with the FDA approval of lotilaner 0.25% ophthalmic solution (Xdemvy, Tarsus). This topical formulation is used twice daily for 6 weeks to kill Demodex folliculorum mites and for the resolution of associated lash collarettes.
Additional prescription medications that can aid in the treatment of blepharitis include antibiotic ointments, as monotherapy or in combination with corticosteroids, for S. Aureus anterior/posterior and angular blepharitis. Topical ophthalmic azithromycin is another option for both the treatment of the associated bacteria, and it has an anti-inflammation effect. Oral antibiotics are also an option for lid margin inflammation and posterior blepharitis, especially when related to ocular/facial rosacea. Typically, a low dose of 40 mg to 50 mg daily of doxycycline for 90 days can be quite effective.
As with all prescription medications, care must be taken to educate patients on possible side effects of use and caution against prolonged self treatment with previously prescribed medications, especially in the case of topical steroids.
• Symptomatic interventions. Finally, we should not minimize the symptom improvement that many patients can obtain with warm (or cool) compresses, humidifiers, moisture seals/goggles, and lubricants. Although I caution patients that these interventions are not addressing the root cause of symptoms, they can yield improvements in symptoms and mild signs, such as improvement in meibomian gland expression, and ocular surface staining.

In-office interventions
The following are in-office lid hygiene tools:
• Blepharoexfoliation. This removes debris and scurf, along with lid margin biofilm, which contains both microorganisms and dead skin cells. It can be done with a specialized device or manually.
CUTOFF BLEPHARITIS FROM COSMETICS
Another patient population for lid hygiene are patients who aren’t exhibiting signs or symptoms of blepharitis, but with whom lid hygiene is still important to discuss. These are patients who are wearing cosmetics on a regular, or even occasional, basis, as well as patients who have lash extensions.
I routinely ask patients whether they wear eye makeup and if so, whether they remove it nightly. Many divulge they do not remove it. Those who say they do, are not using an eye-safe cleanser. As a result, I think it’s imperative we have a conversation with patients regarding safe and effective eye makeup removers and lid cleansers. Many formulations of eye-safe makeup removers are available, including oils, foaming cleanser, and micellar water cleansers.
When it comes to our lash extension-wearing patients, we need to provide education on proper care, so they can avoid significant blepharitis and related DED symptoms. This proper care: a water-based cleanser and brush for daily cleansing of the lids and base of lashes. Water-based cleansers are necessary to prevent oils from loosening the glue used to hold the extensions.
The specialized devices all operate similarly with a rotating cleaner head and the use of some form of cleanser.
Manual blepharoexfoliation can be done using a cleanser and sponge tip applicator or without cleanser, using a debridement tool to manually clean each lid margin until free of scurf and biofilm. Lid cleansers, applicators, and other supplies may come packaged in a kit or may be acquired separately. Some patients benefit from instillation of proparacaine prior to the procedure. My preference is to instill both preservative-free artificial tears, as well as OTC brimonidine 0.025% after the procedure. This is because redness is common immediately after, although it is typically short-lived.
• Low level light therapy. LLLT employs a specific wavelength of light to create antimicrobial and anti-inflammatory effects. Specifically, it is used for the clearing of microorganisms, such as excess staph. bacteria on the lids, as well as Demodex.
• Intense pulsed light. This has been shown to decrease the population of Demodex mites in meibomian glands; the possible mechanism being heating on the meibomian glands above what the mite can withstand. Optimal treatment would include direct treatment of both upper and lower lids, avoiding the eyelashes.3
• Symptomatic interventions. Thermal treatments, meibomian gland expression, and radio-frequency involve heating of the tissues and meibomian glands to yield both improvements in patient symptoms and signs, such as meibomian gland inspissation.
Preparing for multiple treatments
In practice, I have found that many blepharitis patients have both staph. and Demodex, probably because they coexist quite easily: Demodex typically have staph. bacteria living in their very primitive digestive systems, and staph. bacteria thrive on the digestive material and dead skin cells present in Demodex-related lash collarettes. It’s a truly synergistic relationship. As a result, rarely will just one treatment option be enough. OM
References
1. Akl MM. Hypochlorous acid has emerged as a potential alternative to conventional antibiotics due to its broad-spectrum antimicrobial activity. Int J Clin Microbiol Biochem Technol. 2023; 6: 001-004.
2. Tighe S, Gao YY, Tseng SCG. Terpinen-4-ol is the Most Active Ingredient of Tea Tree Oil to Kill Demodex Mites. Translational Vision Science & Technology. November 2013, Vol.2, doi: https://doi.org/10.1167/tvst.2.7.2
3. Zhang W, Cao X, Yang L, Duan Y, Zhang W. Analysis of Treatment Efficacy of Intense Pulsed Light (M22) for Meibomian Gland Dysfunction with Demodex Mites. Clin Cosmet Investig Dermatol. 2023;16:3743-3751. doi: 10.2147/CCID.S435723.




