A 61-year-old African American male presented to the clinic complaining of loss of vision in his right eye that coincided with a hospitalization two months prior for malignant hypertension. He was started on chlorthalidone 50 mg and isosorbide dinitrate, and his blood pressure was well managed at the time of this visit, measuring 123/87 mm Hg. Entrance testing revealed a (+) afferent pupillary defect OD with an abnormal superior visual field OD with finger counting. The left eye had unrestricted and normal visual fields. BCVA measured 20/60 OD and 20/20 OS. Slit lamp biomicroscopy was unremarkable without evidence of neovascularization of the iris and only mild lenticular changes. Gonioscopy was negative for neovascularization of the angle. Intraocular pressure measured 17 mm Hg OD and 16 mm Hg via Goldmann applanation tonometry.
Posterior segment examination revealed venous dilation and tortuosity bilaterally that was only readily visible superiorly OD. The inferior hemisphere of the right retina had sclerosed vasculature including intra-retinal hemorrhages, pre-retinal hemorrhages and anomalous vasculature (both collateral vessels and retinal neovascularization). The macula appeared to be flat without fluid accumulation. Neovascularization of the disc (NVD) was also present. The clinical presentation, entering visual acuity, pupillary reaction and presence of neovascularization were suggestive of an ischemic hemi-retinal vein occlusion OD (Figure 1).
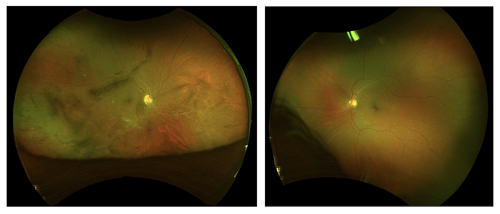
Figure 1.
OCT and OCT-Angiography (OCT-A) were performed to evaluate both the structural abnormalities and extent of ischemia and neovascularization. OCT-A of the vitreoretinal interface confirmed the presence of proliferation and highlighted the extensive disc and retinal neovascularization (Figure 2). Further evaluation of the deep capillary plexus slab highlighted the extensive amount of capillary non-perfusion and anomalous vasculature within the area of occlusion (Figure 3A). The coinciding en-face image brilliantly illustrates not only the neovascularization, but also the venous tortuosity and dilation of retinal vascular system (Figure 3B). A color-coded thickness map was also obtained to complement the angiography and quantify the extent of retinal capillary ischemia (Figure 4). OCT further demonstrated NVD without the presence of macular edema (Figures 5 and 6).
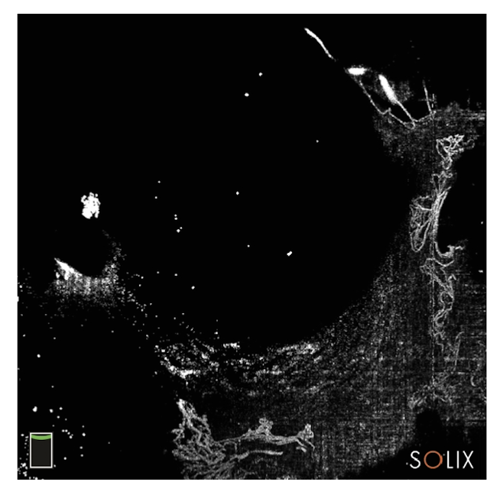
Figure 2.

Figures 3A and 3B.
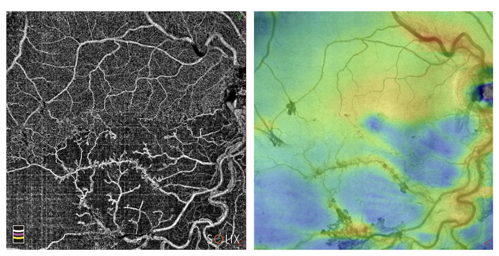
Figure 4.
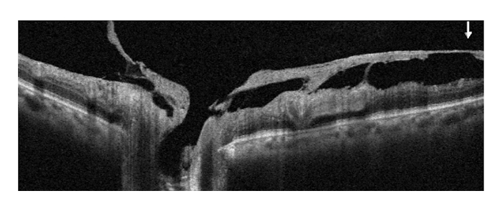
Figure 5.
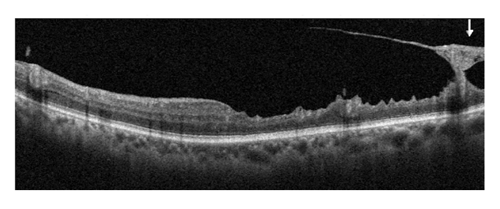
Figure 6.
Retinal venous occlusive disease is commonly encountered in the optometric setting. Multimodal imaging should be used to both confirm diagnoses and provide supplemental information, such as structural findings and vascular status.





