This article was originally published in a sponsored newsletter.
With the new complement cascade inhibition therapies now available for geographic atrophy (GA), we can monitor progression in patients and guide recommendations for medical intervention. We must also have a thorough understanding of coding, billing and restrictions around imaging modalities for treatment and management.
The appropriate ICD-10 codes associated with dry age-related macular degeneration (AMD) include the following, where the x designates laterality; 1 for the right eye, 2 for the left eye, 3 for bilateral1,2:
H35.31x1 for early dry AMD - defined as medium drusen (greater than 63 μm but less than 125 μm) without pigment abnormalities.
H35.32x2 for intermediate dry AMD - defined as large drusen greater than 125 μm, pigment abnormalities or both.
H35.31x3 for advanced dry AMD without subfoveal involvement - GA not involving the center of the fovea.
H35.31x4 for advanced dry AMD with subfoveal involvement - GA that involves the center of the fovea.
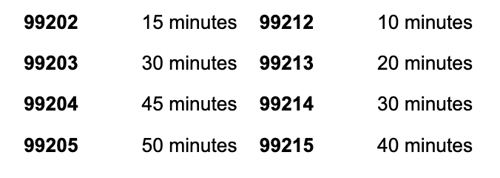
The Current Procedural Terminology (CPT) codes for office-based evaluations and management (E/M) services have also been updated. For 2024, the amount of total physician time on the date of encounter must meet or exceed the designated amount, listed below.
The minimum times for each code are:
These new codes are helpful for managing GA because, in addition to the ocular examination, these patients often require counseling that can be time-consuming. Counseling of GA patients often includes discussions of their daily activities and any struggles that persist after refractive error is best corrected. Primary care optometry can discuss improvements in lighting and contrast of the environment; increased add powers for close work; national programs for free access to braille or auditory books; state-provided occupational therapy services such as orientation and mobility; technology including electronic tablets for texting, emails and reading; and benefits of a referral to low vision services.
Patient education on the new complement cascade inhibition therapies takes time as well and includes the risks, benefits, limitations and goals of treatment with these new therapies. These discussions also involve reviewing serial imaging with patients to determine whether their GA lesion(s) grow over time.
Multimodal imaging of GA is recommended to optimize visualization of the atrophic lesions and assist in monitoring the disease over time.2 The most common imaging for GA includes color fundus photography, fundus autofluorescence (FAF), near-infrared reflectance (NIR) imaging, optical coherence tomography (OCT) and OCT-angiography (OCT-A). Color fundus photography, FAF and NIR imaging all fall under the same CPT code of 92250 (Fundus photography with interpretation and report). This is a bilateral code, so it is used for imaging one eye or both. It is reasonable to repeat FAF and NIR to monitor disease progression because these images can show change that is independent of clinical examination. However, imaging like this can only be repeated and billed if it is necessary to assess disease progression or the advent of new disease, or when planning additional treatments. They cannot be used to photograph the same, unchanged condition. Always document the rationale for repeating these tests and provide an appropriate interpretation and report of the imaging.
It is also important to note that fundus photography is mutually exclusive with code 92134 for OCT/SCODI (scanning computerized ophthalmic diagnostic imaging of the retina), meaning photography and OCT cannot be billed on the same day for GA. In addition, most insurances limit OCT to payments no more than twice per year. If you are monitoring more often than six months, alternate photography/FAF/NIR and OCT/OCT-A per visit to avoid these pitfalls. Like photography, FAF and NIR, there is no separate CPT code for OCT-A. Thus, OCT/SCODI and OCT-A are performed together under the same CPT code of 92134.
Reference(s):
- Ferris 3rd FL, Wilkinson CP, Bird A, et al. Clinical classification of age-related macular degeneration. Ophthalmology. 2013 Apr;120(4):844-851. doi:10.1016/j.ophtha.2012.10.036
- Wu Z, Luu CD, Hodgson LAB, et al. Prospective longitudinal evaluation of nascent geographic atrophy in age-related macular degeneration. Ophthalmol Retina. 2020 Jun;4(6):568-575. doi:10.1016/j.oret.2019.12.011




