This article was originally published in a sponsored newsletter.
Investigators recently attempted to answer this research question in a study with a novel population.1 To be eligible, participants needed at least one eye with previously untreated neovascular age-related macular degeneration (nAMD). Using a prospective observational design, participants were also required to have visual acuity of 20/20 to 20/320.1 After providing consent, the enrolled subjects received a Notal Vision Home OCT device (Notal Vision), which has demonstrated viability as a home-monitoring system in nAMD patients already undergoing treatment.1-3 Patients were instructed to scan both eyes daily.1
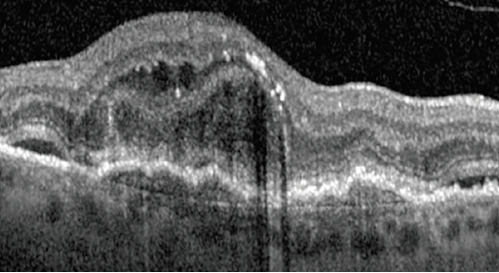
Standard practice nAMD treatment was delivered by participating retina specialists who did not have access to the home OCT data. The presence of fluid detected on in-office scans by a reading center was compared with fluid volumes measured by the Notal OCT Analyzer (NOA) on home OCT images (see Figure 1).1
Primary outcome measures included1:
- The proportion of subjects who met eligibility criteria and participated in daily scanning
- The frequency and duration of scanning
- The proportion of scans eligible for fluid quantification
- Participants’ reported experience with the device
- Agreement between the reading center and NOA fluid determinations
- Characteristics of fluid dynamics
Among 40 participants who met the ocular eligibility criteria, 14 (35%) initiated self-scanning. Planned travel (n = 7, 17.5%) and patient-reported inadequate cell reception for the upload of images (n = 5, 12.5%) were the most frequent reasons for not participating.1 It should be noted that future iterations of the service has included Wi-Fi connectivity and support for patients to transport the devices.
The mean (standard deviation) weekly scanning frequency for the study eye was 6.3 (0.6) and scan duration per eye was 47 (17) seconds. Among 2,304 scans obtained, 86.5% were deemed eligible for fluid quantification.1
All participants agreed that scanning became easier over time, and only one did not want to continue. For 35 scan pairs judged as having fluid by in-office OCT, the NOA detected fluid on 31 scans (89%). For 14 scan pairs judged as having no fluid on in-office OCT, the NOA did not detect fluid on 10 scans (71%). Daily fluid patterns after treatment initiation varied considerably between patients. Fluid >10 nL on Home OCT is considered a threshold for a notification in a future study, and was used in this study to evaluate the performance of the NOA in a single encounter comparison. There was no instance of a NOA fluid level >10 nL when the reading center’s interpretation of the in-office OCT showed no intraretinal or subretinal fluid. Therefore, there were no false positives.1
The investigators concluded that for patients with previously untreated nAMD who initiated home-based OCT, the frequency, quality and accuracy of scanning were sufficient to assess and monitor fluid. Accommodations for travel and Wi-Fi connectivity could improve uptake of the home-based OCT device.1 Novel, self-driven monitoring for retinal diseases represents a significant homework assignment for investigators and patients alike.
Key Clinical Takeaways
- Macular neovascularization is responsible for most severe vision loss in people living with AMD.
- The Notal OCT Analyzer has demonstrated its viability as a home-monitoring system in nAMD patients already undergoing treatment.
- Results of a feasibility trial on treatment-naive patients with nAMD showed the potential value of this new home-monitoring method.
- Future clinical trials using home OCT may one day modify the “treat and extend approach.”
Reference(s):
- Blinder KJ, Calhoun C, Maguire MG, et al. Home OCT imaging for newly diagnosed neovascular age-related macular degeneration: a feasibility study. Ophthalmol Retina. 2024 Apr;8(4):376-387. doi:10.1016/j.oret.2023.10.012
- Liu Y, Holekamp NM, Heier JS. Prospective, longitudinal study: daily self-imaging with home OCT for neovascular age-related macular degeneration. Ophthalmol Retina. 2022 Jul;6(7):575-585. doi:10.1016/j.oret.2022.02.011.
- Blinder KJ. More homework for patients with macular degeneration? JAMA Ophthalmol. 2024 Apr 25. doi:10.1001/jamaophthalmol.2024.1050 [Online ahead of print].




