Contact lens dropout is a challenging reality in any contact lens practice. Both the eye care provider and patient expend time, energy, and resources to find a contact lens option that can satisfy the patient’s visual and comfort needs. When contact lens dropout results, it can feel like a defeat for everyone involved. Dropout rates have stayed relatively stable over the last several years, which is why it’s important to consider revisiting the issue and a new approach to deterring it.1,2,3
It is well-established that most contact lens dropout is due to “discomfort.”3 Discomfort can be caused by an incompatibility between the contact lens and the ocular surface, or it may be caused by a visual mismatch between the power of the lens and the patient’s refractive needs.4 For many patients, discomfort is likely a sensation caused by multiple factors that lead to a singular result of discontinuation of contact lens wear.
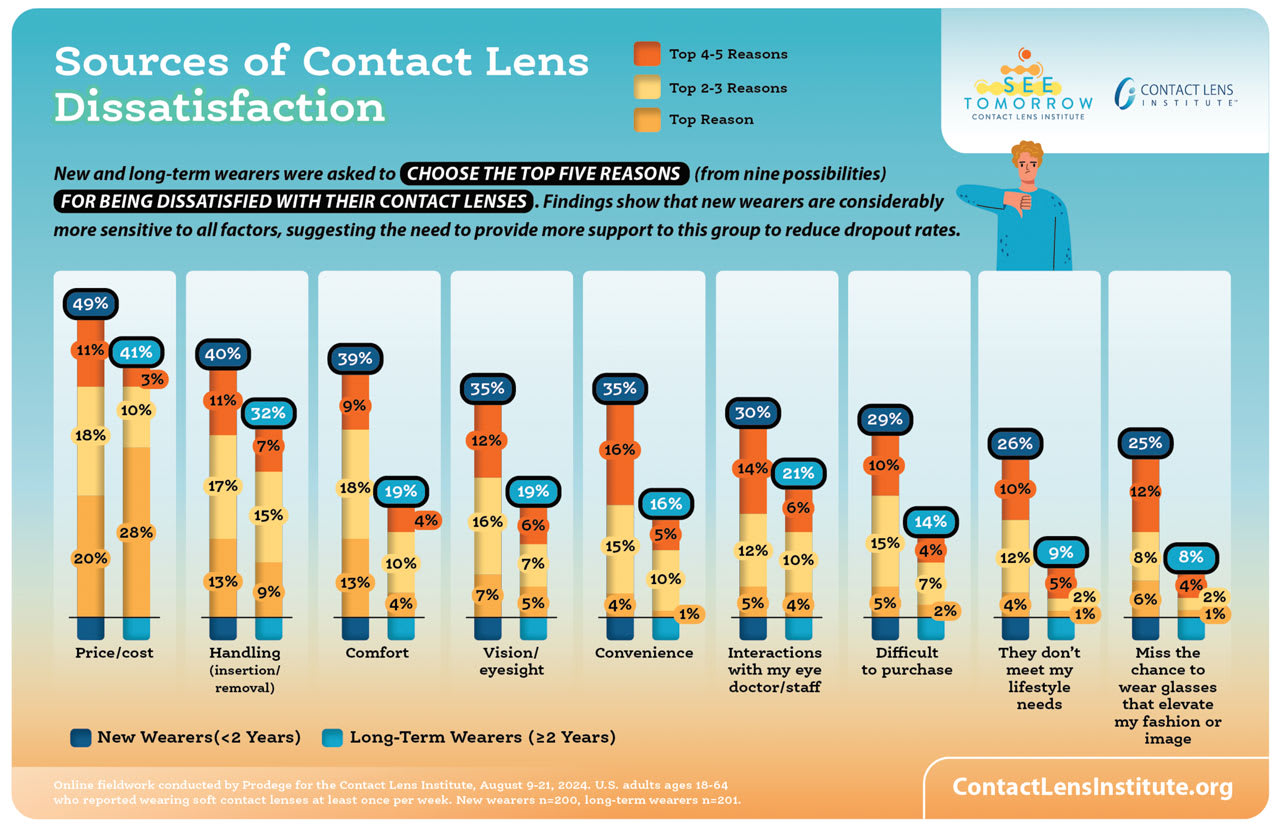
That said, discomfort isn’t the only reason patients might discontinue contact lens wear. A recent report by the Contact Lens Institute reveals that, while discomfort was a primary reason for contact lens dissatisfaction, other factors, such as cost, lens handling issues, convenience, and visual factors influence dissatisfaction with contact lens wear.5
The many intermingling and compounding factors that impact a wearing experience must be considered to prevent dropout. Therefore, the eye care provider needs to adopt a practice of acknowledging the products available, while considering each patient’s visual and lifestyle goals to prevent contact lens dropout and retain lifelong, loyal patients.
Read on for the strategies I’ve used that you can implement in your practice to prevent dropout.

1. Use your influence
It’s easy to assume that a patient will ask about contact lenses if they are interested and, similarly assume that a patient on the brink of dropout will let us know.
More often, however, that patient is waiting for us to tell them there is a problem or suggest a solution.
In fact, a recent study shows that just 30% of patients who eventually dropped out of contact lens wear were offered an alternative option.6 This highlights the importance of our opinion and recommendation, regardless of the patient’s perceived level of satisfaction with their current lenses.
Considering the impact of the eye care provider’s influence, it’s important they take advantage of the opportunity they have to prevent dropout while the patient is in their chair. Obviously, if the patient is expressing concerns with comfort or vision, the eye care provider will discuss the patient’s options for changing lens designs or modalities. What’s just as crucial, however, is to discuss alternative lens options with those wearers not reporting any specific complaints. This means broaching new product options that are relevant to the patient’s lifestyle and refractive status each year. In addition to solving a potential issue, such as end-of-day ocular dryness that the patient has gotten used to or just accepted, this conversation reminds the patient of the value of checking in with us. What’s more, if the patient experiences contact lens problems at any time after the exam, they will remember that we can offer solutions.
For example, should a patient present expressing concern about the cost of upgrading to a daily disposable modality, the eye care provider and/or their staff can use in-practice time to break down the daily costs of daily disposable modalities compared to monthly modalities, pointing to incidental costs, such as lens solutions and lens cases.
Also, we or our staff can emphasize the added value of convenience and the patient’s ability to communicate with the practice if/when any issues occur when the patient gets their prescriptions and contact lenses from us.
The bottom line is that the eye care provider demonstrating all the ways they can help the patient if they are not satisfied can preempt potential contact lens discontinuation.
2. Optimize the ocular surface
While incompatibility between the ocular surface and a contact lens is not the only reason for dropout, it does play a primary role in a wearer’s comfort. Therefore, we should assess the ocular surface carefully before initiating a fit or when troubleshooting discomfort.
It’s been reported that patients who have low tear break-up times, low tear volume, and corneal and conjunctival staining are more likely to dropout of contact lens wear compared to those without these findings.7 Further, it has been reported that successful contact lens wearers have less meibomian gland tortuosity and gland plugging than discontinued wearers.1
When signs of ocular surface dryness are observed, no matter how mild, we should educate the patient on strategies for optimizing the health of their ocular surface and its interaction with a contact lens.
Specifically, talk to patients about the importance of proactive lubrication with artificial tears and suggest the use of products that are appropriate for the patient’s lens brand and modality. Also, demonstrate practices for proper lid hygiene for meibomian gland support. Finally, let the patient know that if they experience dryness or discomfort symptoms that cause them to decrease their wearing time, they can return to the practice to address those issues.
3. Prioritize vision
In contact lens wearers, symptoms of visual discomfort are easily misunderstood.4 When patients complain of discomfort, we may assume that it is due to an ocular surface and contact lens issue. Discomfort, however, can be caused by visual issues that lead to eyestrain, fatigue, and ocular discomfort.
Consider this: The primary reason for dropout in neophyte contact lens wearers has been dissatisfaction with vision.2 Similarly, presbyopic contact lens wearers who have discontinued wear have cited vision as often as discomfort as a reason for contact lens dropout.8
It is crucial that the eye care provider choose the best power and optical design for each unique patient. This starts with a fresh refraction every year. Regardless of how stable a patient’s refractive status has been or how well they are seeing in their current contact lenses, we should repeat the refraction annually and compare it to their contact lens power. Over/under correction of sphere power, for instance, can cause visual fatigue and/or strain at near. Additionally, the eye care provider should consider the patient’s age and presbyopic status to ensure they are wearing the optimal sphere power for their distance and near needs.
Next, we should consider astigmatic options. About half of all contact lens wearers have 0.75 D or more of astigmatism in at least one eye.9 Patients who have low or mild amounts of astigmatism actually prefer toric to spherical contact lenses options.10 These patients have improved visual acuity and visual function in both low light and glare conditions when corrected with a toric contact lens option.11,12 Additionally, soft toric lenses improve symptoms of eyestrain and fatigue in low astigmats.10
Finally, we should address presbyopia and pre-presbyopia. As multifocal options continue to im- prove and expand, it can be impactful to initiate a multifocal early in a patient’s presbyopic journey or even before they begin experiencing symptoms of near blur. Pre-presbyopes have been shown to prefer multifocal to spherical options,13 even before they turn 40.
4. Follow up
If we do not follow-up with our contact lens wearers, we may never know that they dropped out of lens wear. It is possible that a new wearer leaves the office with trial lenses and never returns because they weren’t satisfied with the vision or comfort and they wrongly assume the problem can’t be solved.
Regular follow up obviously means implementing patient recall systems, but it also means that, especially in the time immediately following the dispensing of trial lenses and/or the finalization of the contact lens prescription, the eye care provider follows up to ensure the patient is satisfied with the contact lens option they have. Depending on the patient, this follow-up could be a quick in-person check-up or a text/email/phone call from a staff member.
This communication or in-office touchpoint should allow the patient to give feedback on their contact lens-related experiences, such as comfort, vision, and overall satisfaction. This is also a great time for us to ask how at-home lens handling is going or whether the modality chosen is fitting the patient’s expectations and lifestyle needs. Keeping the lines of communication open in the crucial days and weeks after dispensing, which is when the patient is likely deciding whether they should continue with the contact lenses, is key for identifying any issues that might lead to dropout and solving them. Addressing those issues in response to patient feedback fosters loyalty in the patient and can prevent dropout.
A multifaceted approach
There is not one magic step or fix for preventing contact lens dropout. Eliminating dropout requires a thorough understanding of why patients dropout and an acknowledgement that dropout is often caused by multiple factors. Addressing all these factors in a cohesive, efficient way that involves open communication with the patient will lead to long-term, satisfied wear for the patient and practice. OM
References:
1. Pucker AD, Jones-Jordan LA, Marx S, et al. Clinical Factors Associated with Contact Lens Dropout. Cont Lens Anterior Eye. 2019;42:318-24. doi: 10.1016/j.clae.2018.12.002. Epub 2018 Dec 8.
2. Sulley A, Young G, Hunt C, McCready S, Targett MT, Craven R. Retention Rates in New Contact Lens Wearers. Eye Contact Lens. 2018;44 Suppl 1:S273-S282. doi:10.1097/ICL.0000000000000402.
3. Pucker AD, Tichenor AA. A Review of Contact Lens Dropout. Clin Optom (Auckl). 2020;12:85-94. Published 2020 Jun 25. doi:10.2147/OPTO.S198637
4. Rueff EM. Visual discomfort and contact lens wear: A review. Cont Lens Anterior Eye. 2023;46(4):101872. doi:10.1016/j.clae.2023.1018725.
5. Contact Lens Institute (CLI). Disrupting the Dropout Dilemma: Practical Steps to Keep Patients in Contact Lenses. Fall 2024. https://www.contactlensinstitute.org/resources/see-tomorrow-disrupting-dropout (Accessed Nov.8, 2024.)
6. Sulley A, Young G, Hunt C. Factors in the success of new contact lens wearers.
Cont Lens Anterior Eye. 2017;40(1):15-24. doi:10.1016/j.clae.2016.10.002
7. Giannaccare G, Blalock W, Fresina M, Vagge A, Versura P. Intolerant contact lens wearers exhibit ocular surface impairment despite 3 months wear discontinuation. Graefes Arch Clin Exp Ophthalmol. 2016;254(9):1825-1831. doi:10.1007/s00417-016-3400-4.
8. Rueff EM, Varghese RJ, Brack TM, Downard DE, Bailey MD. A Survey of Presbyopic Contact Lens Wearers in a University Setting. Optom Vis Sci. 2016;93(8):848-854. doi:10.1097/OPX.0000000000000881.
9. Young G, Sulley A, Hunt C. Prevalence of astigmatism in relation to soft contact lens fitting. Eye Contact Lens. 2011;37(1):20-25. doi:10.1097/ICL.0b013e3182048fb9.
10. Cox SM, Berntsen DA, Bickle KM, et al. Efficacy of Toric Contact Lenses in Fitting and Patient-Reported Outcomes in Contact Lens Wearers. Eye Contact Lens. 2018;44 Suppl 1:S296-S299. doi:10.1097/ICL.0000000000000418.
11. Black AA, Wood JM, Colorado LH, Collins MJ. The impact of uncorrected astigmatism on night driving performance. Ophthalmic Physiol Opt. 2019;39(5):350-357. doi:10.1111/opo.12634.
12. Richdale K, Berntsen DA, Mack CJ, Merchea MM, Barr JT. Visual acuity with spherical and toric soft contact lenses in low- to moderate-astigmatic eyes. Optom Vis Sci. 2007;84(10):969-975. doi:10.1097/OPX.0b013e318157c6dc.
13. Rueff EM, Jones-Jordan LA, Bailey MD. A randomised clinical trial of multifocal contact lenses and contact lens discomfort. Ophthalmic Physiol Opt. 2021;41(1):93-104. doi:10.1111/opo.12761.




