Scleral lenses can dramatically improve quality of life by restoring the ability to drive and work for patients who have advanced keratoconus (KCN), and ease pain for those who have debilitating ocular surface diseases, such as dry eye disease. As someone who has been fitting scleral lenses for 15 years, I have also experienced the many benefits scleral lenses bring to a practice. Yet, the most rewarding aspects of providing scleral lenses are the patient relationships and loyalty they create. Patients are grateful for the improvement in their vision, ocular comfort, and quality of life.
For many optometrists, fitting patients in these life-changing lenses still brings trepidation. This worry is due to design selection, ocular surface lens alignment, and insertion and removal education, all of which can create extended chair time.
In this article, let’s remove some of the mystery from the prescribing process and build strategies that can make it easier to learn and incorporate this service. By embracing these skills, optometrists can increase their support of a range of patients, from those who have mild symptoms, to those who struggle with daily pain or poor vision.
Seek resources
There are many opportunities to learn scleral lens-fitting skills; specifically in hands-on wet labs, lecture halls, and virtual settings. Lecture-based and hands-on education is often given at meetings, and many scleral lens manufactures can provide in-office training when requested. The Scleral Lens Education Society also provides entry-level virtual education on scleral lens prescribing. Follow the SLS here: https://sclerallens.org/
Identify best candidates
According to the SCOPE study1, irregular corneas, such as those that have KCN, are the primary indication for scleral lenses. Ocular surface diseases are the second most common indication for scleral lens wear.2
Because scleral lenses are so customizable, patients who have mild-to-severe disease are candidates for lens wear, and when combined with corneal collagen cross-linking, patients with KCN may delay or even negate the need for a corneal transplant.3
Some patients may be more challenging to initially fit, such as patients who have deep-set orbits or strong blink reflexes. Consider having several diameters of scleral lenses, as well as a variety of insertion and removal tools to allow for trialing various techniques.
Schedule strategically
Optometrists new to scleral lens fitting can schedule their first scleral lens appointments when they are least likely to feel rushed. Some make these appointments the last of their day. Others block a designated amount of time each week for only these patients. It’s also helpful to have a designated flow for needed testing to streamline the experience for patients and technicians.
Use technology
Corneal topography provides the patient’s cornea size and shape, and aids in diagnosis. This information is important, as it influences the chamber size, lens profile, and overall diameter of a scleral lens. For example, post-surgical eyes will have a different shape and depth compared to eyes that have KCN.
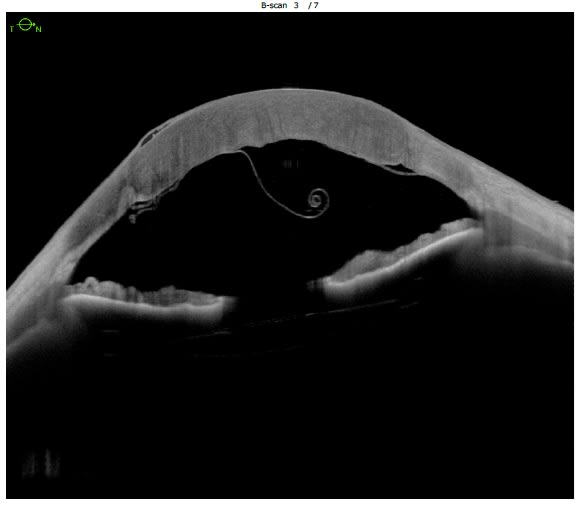
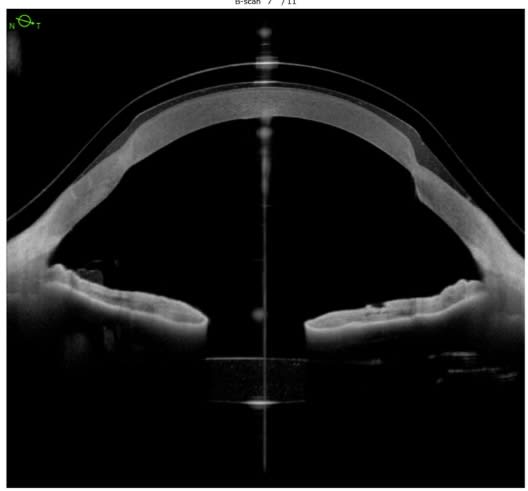
A well-fitting scleral contact lens will clear the cornea and limbus by precise amounts, and land evenly on the sclera. Anterior-segment (AS)-OCT gives precise views of central and limbal clearance. Aligning a scleral lens chamber to the peri-limbal area can be a challenging part of a fitting, especially in eyes that are significantly irregular in shape due to their post-surgical status. An example: Those that have undergone radial keratotomy or corneal transplantation. An AS-OCT can assist in modifications that are difficult to assess in the slit lamp.
Slit lamp photography is another tool for designing and troubleshooting scleral lenses. The images and videos can be reviewed and shared with laboratory consultants, which enables them to provide their optimal guidance on parameter changes for simple or complex cases.
Recruit interested staff
Some team members will enjoy working with your scleral lens patients more than others. Foster this interest in those team members who enjoy a challenging case yet show high levels of empathy and patience. These team members can be a great asset to this service, as they have the patience to obtain a good quality cornea scan, answer patient questions, and assist with insertion and removal trainings.
Ready for more?
Once ODs begin to see success in scleral lens prescribing, high-level education is routinely offered at annual meetings hosted by the Global Specialty Lens Symposium and the International Congress of Scleral Contacts, among other organizations. These meetings are excellent opportunities to connect with colleagues and find a mentor. OM
Lere more about GSLS here: https://gslsymposium.com/live/1/page/1?itm_source=event_banner&itm_event_id=1
Learn more about ICSC here: https://www.icscmeeting.com/
References:
1. Schornack MM, Fogt J, Nau A, Nau CB, Harthan JS, Cao D, Shorter E. Scleral lens prescription and management practices: Emerging consensus. Cont Lens Anterior Eye. 2023;46(1):101501. doi: 10.1016/j.clae.2021.101501.
2. Ruiz-Lozano RE, Gomez-Elizondo DE, Colorado-Zavala MF, Loya-Garcia D, Rodruguez-Garcia A. Update on indications, complications, and outcomes of scleral contact lenses. Med Hypothesis Discov Innov Ophthalmol. 2021;10(4):165-178. doi: 10.51329/mehdiophthal1435.
3. Koppen C, Kreps EO, Anthonissen L, Van Hoey M, Dhubhghaill SN, Vermeulen L. Scleral Lenses Reduce the Need for Corneal Transplants in Severe Keratoconus. Am J Ophthalmol. 2018;185:43-47. doi: 10.1016/j.ajo.2017.10.022.




