Optometrists widely utilize and value optical coherence tomography (OCT) for its clinical importance in aiding in the diagnosis and management of retinal pathology. Anterior segment (AS)-OCT is proving to be an equally important tool in the evaluation of the ocular surface and in the fitting and management of specialty contact lenses.
Here, I explain how so.
Tear Volume Measurement
AS-OCT enables clinicians to capture and measure an image of the tear meniscus. This is important, as both the tear meniscus height and area reveal the difference between healthy and dry eye disease patients.1 Thus, measuring tear volume is an important component of the pre-fitting contact lens work-up. The tear meniscus appears as a wedge of tear film between the lower lid margin and ocular surface via AS-OCT. Using the AS-OCT’s measurement software, we can analyze tear meniscus height, tear meniscus depth, and tear meniscus area.
Keratoconus Management
With its precise corneal imaging, AS-OCT can aid in the early detection of keratoconus (KCN) and help us assess the extent of ectasia, severity of thinning, and associated focal Descemet’s membrane irregularities.2 The technology may be particularly useful for optometrists who don’t have access to Scheimpflug-based corneal tomography. This is because both Scheimpflug-based imaging and AS-OCT provide comparable readings with a good agreement regarding corneal pachymetry with accurate identification of KCN eyes and healthy ones. A caveat: Researchers caution that due to the significant difference in keratometry readings between both devices, it is inadvisable to use the 2 devices interchangeably.3
Corneal Gas Permeable Lens Fits
AS-OCT can aid in the fitting of all types of rigid lenses. For example, it allows for the precise measurement of the apical clearance of corneal gas permeable lenses. Also, it can be used to measure the clearance and “lift” of reverse curves and edges when fitting orthokeratology lenses.
My Go-to Use
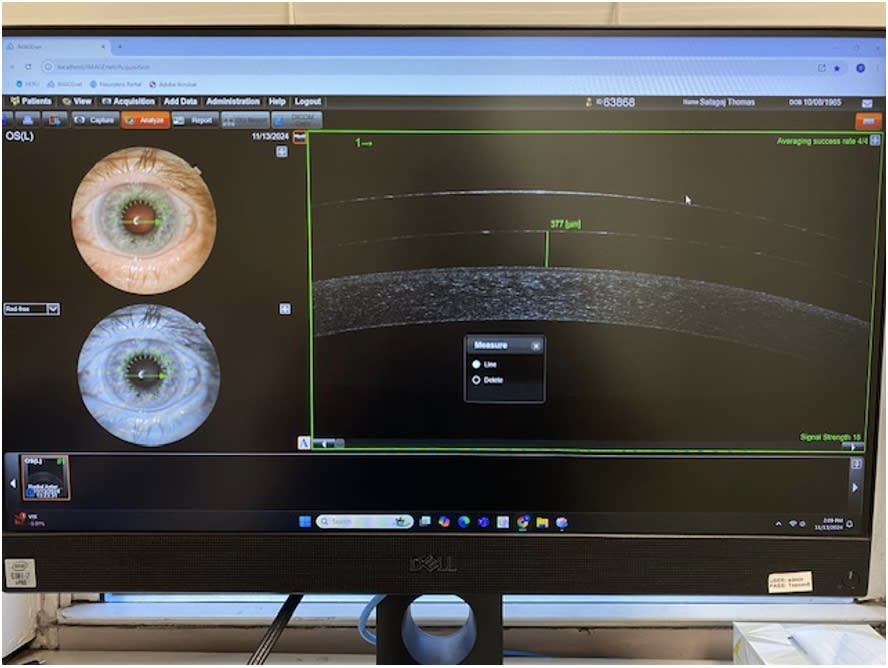
I most commonly use AS-OCT for the fitting and evaluation of scleral lenses. This is because it allows for the precise evaluation of the central corneal vault, limbal clearance and scleral landing (ie, edge design). My approach is to capture images upon fitting and again at the first follow-up visit after the patient has worn the lens
for more than 4 hours. I look for a minimum of 150 μm of corneal clearance, and 60 to 80 μms of limbal clearance. By obtaining scans at different gaze directions, I then assess whether the lens edge is consistently aligned with the sclera or there are areas of impingement or lifting. I then make fitting alterations, such as increasing or decreasing the vault or haptic toricity based on both these measurements and my slit lamp examination. OM
Pro-tips for manual tear meniscus height measurement
- Capture image of vertical section of the inferior tear meniscus and measure from the upper corneo-meniscus junction (i.e. where the tear film meets the cornea to the lower eyelid meniscus junction)
- Rotate the image 90° and magnify for easier measurement.
- Use the software-measuring tool to draw a line connecting the 2 points. (The software will display the length of the line.)
References
- Meixiao Shen, Jianhua Li, Jianhua Wang, Huixiang Ma, Chunyan Cai, Aizhu Tao, Yimin Yuan, Fan Lu; Upper and Lower Tear Menisci in the Diagnosis of Dry Eye. Invest. Ophthalmol. Vis. Sci. 2009;50(6):2722-2726. https://doi.org/10.1167/iovs.08-2704.
- Matalia H, Swarup R. Imaging modalities in keratoconus. Indian J Ophthalmol. 2013 Aug;61(8):394-400. Doi: 10.4103/0301-4738.116058. PMID: 23925322; PMCID: PMC3775072.
- Said, O.M., Kamal, M., Tawfik, S. et al. Comparison of corneal measurements in normal and keratoconus eyes using Anterior Segment Optical Coherence Tomography (AS-OCT) and Pentacam HR topographer. BMC Ophthalmol 23, 194 (2023). https://doi.org/10.1186/s12886-023-02946-w




