Because certain ocular conditions, such as myopia, retinopathy of prematurity, and strabismus, are common in pediatric patients, primary care optometrists should make a point of actively seeking these patients. What’s more, diagnosing and managing these patients effectively results in changing a young patient’s life for the better, garnering additional referrals, and, in some cases, retaining these patients for life. All that said, we know that the thought of examining infants, toddlers, and elementary school students can be anxiety provoking for some optometrists due to these patients’ immaturity.
Therefore, this article provides the specific action steps and tricks we have used that have alleviated this anxiety.
These action steps and tricks are based on patient population, cognitive ability, and comfort to ensure the efficient acquisition of usable data. Additionally, we recommend the optometrist be amenable to switching up their typical testing order, prioritizing gleaning information that may be more pertinent to a chief complaint. Lastly, we suggest the OD inform the caregiver at the exam’s start that additional exams may be necessary to complete the evaluation. (See “Establishing Patient Rapport,” p.24)
OK, now let’s get into it.
Visual Acuity: Choose Appropriate Optotypes
• Infants. Visual acuity should be taken with Cardiff or Teller acuity cards. An optokinetic drum can be an alternative for gross acuity measurement in very young infants. If an optokinetic drum is not available, fixation-and-follow techniques can be employed as another gross measurement of acuity by using a penlight or light-up target and moving it in an H-pattern in front of the child.
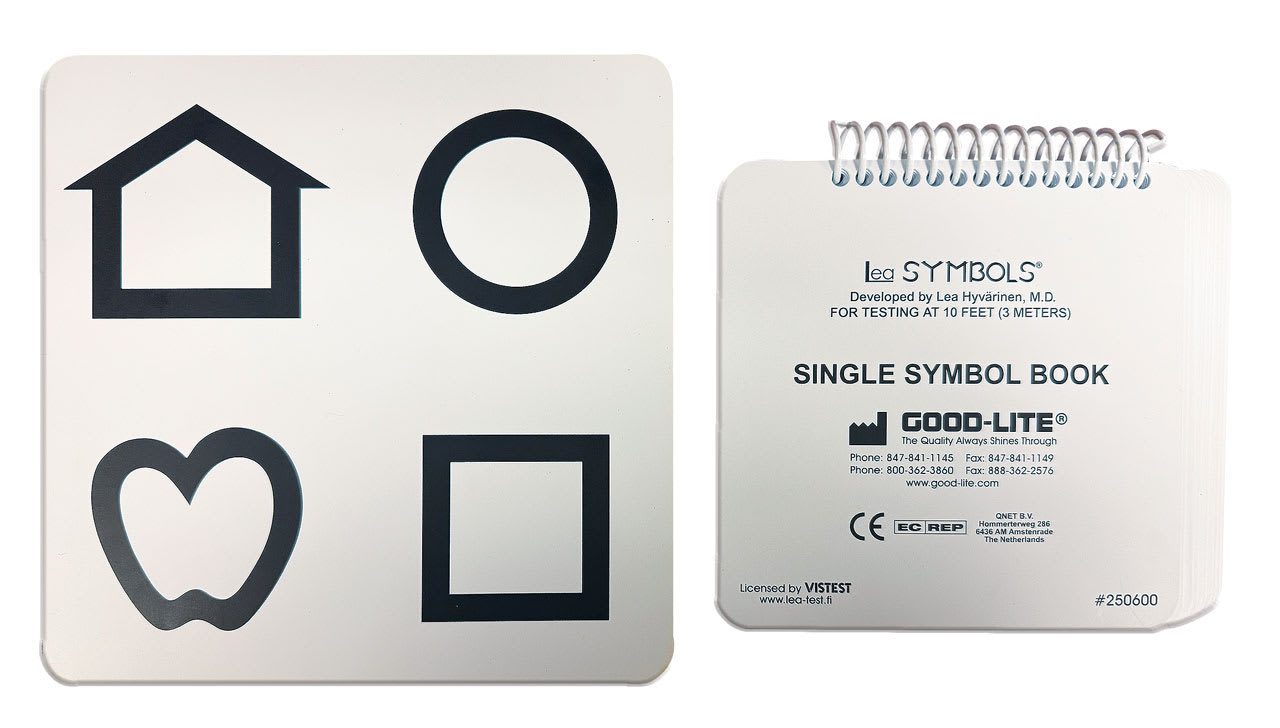
• Toddlers. Cardiff, Lea, Allen, or HOTV cards are effective here. Cardiff cards contain well-known objects (boat, duck, etc.). Lea cards contain shapes (circles, squares, etc.), HOTV cards (or a chart) contain the letters “HOTV,” requiring the toddler to match the letters as their eyes travel down the chart. Allen cards may also be used, and contain familiar images (birthday cake, birds, telephone, etc.) to the patient. All these cards are effective, as this patient population is verbal. Crowding bars or single-target optotypes should be used to eliminate confusion.
• Elementary school children. These young patients do well with Snellen letter optotypes, as they know their alphabet and are learning to or can read. If these patients do not yet know all their letters, Lea cards work well. Something else to keep in mind: Using single-letter optotypes for patients who have amblyopia provides less visual noise and, thus, more accurate visual acuities, as these optotypes reduce the crowding effect.
Color Vision: A Simple Tool and More
• Infants. N/A
• Toddlers. Color Vision Testing Made Easy is a simple tool that can test color vision in these patients.
• Elementary school children.
The Ishihara color vision booklet can be used. If there is a deficit in color vision based on Ishihara, the patient should undergo further testing, including the Farnsworth D-15 Color Blind Test.
Refraction: Employ the Retinoscope/Autorefractor
• Infants and toddlers. Retinoscopy enables the assessment of refractive error in infants and toddlers because the device overcomes the unstable fixation and accommodation that is often characteristic of these populations. We employ loose lenses or skiascopy bars in these patient populations. Small pupillary distance trial frames are also available. When retinoscopy is challenging or the infant or toddler isn’t cooperating, we use a portable, handheld autorefractor to acquire the refractive error.
To keep the infant or toddler’s attention, we use a toy that lights up and makes noise. As each child’s interest can differ, we recommend having several such toys on hand. Digital acuity charts can contain movie options to capture these young patients’ attention as well. Asking their parent/caregiver about their child’s favorite TV show and having the parent/caregiver’s phone to play it for them is also effective. If the parent needs to hold the child on their lap for the exam, a technician can be on hand to help.
• Elementary school children. Accommodation and fixation can still be poor/unstable in this patient population, so employing retinoscopy makes sense. However, autorefractors can also be utilized, as these patients tend to be able to sit comfortably behind this device, follow directions, and keep their attention on the images (buildings, balloons, etc.) presented. In cases where the child’s accommodation or binocular system is unstable, out-of-phoropter trial frame refractions are preferred. Cycloplegic refractions are indicated in cases of reduced visual acuity.

Binocularity: Use a Penlight and More
• Infants and toddlers. A penlight or transilluminator to observe corneal light reflex, both monocularly and binocularly, can obtain Hirschberg or angle kappa measurements.
Additionally, an occluder for the cover test to diagnose tropia is used. Patient resistance to occlusion is often a sign of poor vision in one eye. That said, an occluder may intimidate the patient, so using a thumb as an occluder can be a good alternative in these cases. A stereoacuity booklet, which features targets (cat, star, car) of different disparities, aids in assessing depth perception in toddlers.
• Elementary school children. Baseline testing in this patient population should include occlusion, visual acuity, stereoacuity, and near point of convergence testing. However, performing ocular alignment, stereoacuity, accommodative, and oculomotor testing prior to refraction is not enough to ensure the patient obtains optimal vision. Therefore, we recommend building a trial frame and testing these skills post-refraction as well. If a significant refractive correction is found or a large change made, retesting should be considered. Due to this population’s short attention spans, having the child return to assess the impact of the refractive correction on their visual system may make sense.
Stereoacuity testing can be taken using the Preschool stereo test, PASS, or Randot stereo books. Stereoscopic glasses enable the assessment of both global and local stereopsis with age-appropriate targets. The presence of global stereopsis signifies bifoveation and, therefore, binocularity.
Donder’s Push Up or Pull Away Methods can evaluate accommodative amplitudes in this patient population. For the Push Up method, we move a line of letters progressively toward each patient’s eye until they report blur. For the Pull Away Method, we place the line of letters directly in front of the patient’s eyes and progressively move it away until the patient says the line of letters become clear.
The Monocular Estimation Method (MEM) can assess the patient’s accommodative posture after their refraction. Specifically, the patient focuses on an age-appropriate card while wearing loose lenses or skiascopic bars, while we monitor the patient’s retinoscopic reflex. An abnormal lag or lead of accommodation reveals accommodative dysfunction and may warrant an add for near tasks.
Monocular and binocular accommodative facility testing may be indicated in the presence of other abnormal accommodative findings, such as reduced amplitudes, abnormal accommodative posture, or in children who complain of blur when switching their focus from the board and their school desk.
The NSUCO/Maples Oculomotor Test can assess gross eye movements. Specifically, the optometrist can observe the patient’s saccades by asking the patient to move their eyes back and forth between 2 sticks without the patient moving their head or body to do so. To monitor the patient’s pursuits, the OD moves one of these sticks or a penlight or transilluminator up down, left, and right directly in front of the patient to see whether the patient can follow it without issue. If the patient’s saccadic eye movements are suspect, the Developmental Eye Movement Test or the King-Devick Test can provide further insight. The former requires the patient to read horizontal and vertical letters aloud, while the optometrist keeps track of the time taken to accomplish each, along with any mistakes. This test aids in determining an oculomotor dysfunction or if other issues are present, like Random Automated Naming (RAN). RAN is closely related to issues with reading, such as visual-processing speed and fluency. The King-Devick Test requires the patient to name rapidly changing single-digit numbers within 2 minutes to determine eye movement, attention and language-function impairment, which signal a concussion if reduced compared to baseline. Age-based normative values are available for these tests, giving insight into the child’s oculomotor system. Patients with poor school performance should be tested for oculomotor dysfunction.
Anterior Segment: Use a 20 D lens and a Penlight
• Infants and toddlers. A 20 D lens, a penlight, or a direct ophthalmoscope can evaluate anterior segment health. To maintain fixation, a light-up toy or a video can be used.
• Elementary school children. Slit lamp should be utilized to evaluate the anterior segment. Having the child sit on their knees or stand on the floor can help if positioning is difficult in smaller children.
Posterior Segment: Employ Toys or a Video
• Infants and toddlers. Light-up toys or a video can maintain fixation in these patient populations while a binocular indirect ophthalmoscope (BIO) is used. In the infant and toddler population, we often get just a clear view of the optic nerve and macula. This is because peripheral retinal disease is not common in these patients, unless patient history or family history suggests otherwise. Posterior segment evaluation may require squatting, kneeling on the floor or another dynamic movement to achieve views. The caregiver can help in redirecting a squirming child, or guiding fixation.
• Elementary school children. Attaching stickers to the slit lamp help maintain fixation during the 90 D evaluation. Playing an interesting video from a mobile device can also guide fixation in different gazes on BIO.
Fulfillment
By implementing the action steps discussed above, we have found that seeing pediatric patients is both personally and professionally fulfilling, vs daunting. We hope you have the same experience in trying them. OM
Special thanks to Dr. Miki Zilnicki for using her background in pediatric optometry to peer review this article.





