Patients who have diabetes require special considerations when managing their contact lens wear. This is because diabetes may result in prolonged periods of compromised corneal epithelium from reduced corneal sensitivity and slower corneal healing, increasing the risk of infection.1Additionally, this metabolic disease increases the likelihood of dry eye disease (DED), which may further the possibility of pathological changes to the ocular surface, including neurotrophic keratitis.1 The good news: optometrists can reduce the possibility of these complications by following these recommendations.
Fitting Single-Use Lenses
Single-use lenses (prescription permitting) are ideal for patients who have diabetes, as they are replaced daily. I do not give these patients the option of reusable lenses.
This is how I communicate the health benefits of these lenses to these patients: “Because diabetes can affect your resistance to infection and may increase ocular dryness, I’m prescribing single-use contact lenses, which are the safest.”
Emphasizing Fastidious Hygiene
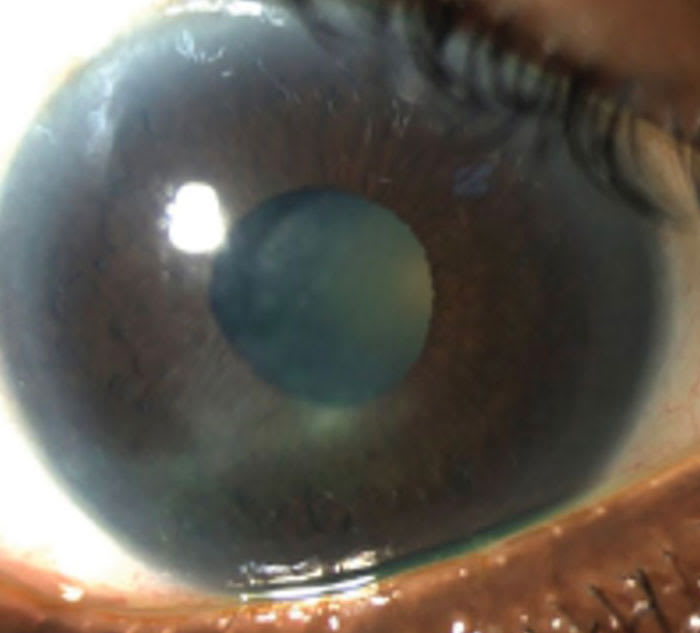
Regardless of lens modality, I educate all patients on the importance of handwashing prior to both lens insertion and removal. Even though single-use lenses are ideal for patients who have diabetes, I know all too well that this lens modality can also be abused. Therefore, I educate these patients thatwear exceeding 12 hours may contribute to the increased risk of a degenerative eye disease (ie, neurotrophic keratitis) due to reduced oxygen to the cornea. Additionally, I stress that showering or swimming while wearing lenses as well as washing lenses with tap water can increase infection to the cornea (ie, microbial keratitis), which can lead to blindness.2 Pro tip: At follow-up appointments, ask patients, “Do you wear your lenses more than 12 hours per day?” and “How often do you fall asleep in your lenses?”
Assessing Ocular Surface Health
Half of patients who have type 2 diabetes also have DED symptoms and the higher the hemoglobin A1C (HBA1C) values, the higher the rate of dry eye disease.1 As a result, I perform a comprehensive ocular surface evaluation prior to fitting these patients in lenses. My basic work-up: slit lamp evaluation with vital dyes, measurement of tear film break-up time, diagnostic meibomian gland expression, and analysis of tear prism thickness. If the patient has DED, I prescribe treatment and delay or deny fitting, pending acceptable treatment results.
Ramping up Recall
Given the predisposing ocular issues of diabetes, I create an appropriate recall schedule.I arrive at this schedule byfactoring in diabetes severity, retinal health status, and contact lens wearing habits. As an example, for those patients wearing contact lenses whose ocular health remains excellent, I recommend a semi-annual progress check. Also, I continue to perform their regularly scheduled internal ocular evaluations, consistent with the presence and/or severity of any retinal pathology. These exams may or may not coincide with their contact lens progress evaluations. I explain to the patient the clinical differences in purpose between these appointments to ensure their understanding and compliance.
Diligence is Key
As is the case with patients who do not have diabetes, patients who have this metabolic disease can wear lenses successfully.I have found that the key toensuring healthy contact lens wear in our patients who have diabetes is diligence regarding the above. OM
References
1. Zhang X, Zhao L, Deng S, Sun X, Wang N. Dry Eye Syndrome in Patients with Diabetes Mellitus: Prevalence, Etiology, and Clinical Characteristics. J Ophthalmol. 2016;2016:8201053. doi:10.1155/2016/8201053.
2. Stellwagen A, MacGregor C, Kung R, Konstantopoulos A, Hossain P. Personal hygiene risk factors for contact lens-related microbial keratitis. BMJ Open Ophthalmol. 2020;5(1):e000476. Published 2020 Sep 8. doi:10.1136/bmjophth-2020-000476.




