Case Presentation
A 58-year-old female patient presented with a decades-long history of fluctuating vision following radial keratotomy (RK) performed in 1996 for high myopia. Despite numerous attempts at visual rehabilitation—including 6 separate contact lens fitting efforts by different providers over the previous 10 years—she continued to struggle with blurred, unstable vision. Eyeglasses provided minimal benefit, and the patient reported increasing difficulty with her day-to-day visual tasks. She was otherwise healthy, took no systemic medications, and had no ocular history apart from her high myopia prior to RK.
On slit lamp examination, the anterior segment appeared largely unremarkable, with the exception of expected RK scars, mild dry eye, and central iron deposition at the level of the epithelial basement membrane in both eyes. The left cornea also exhibited a subtle central haze.
Given the poor performance of prior contact lens modalities, a scleral lens was selected for trial fitting. The initial fit was acceptable, and lenses were ordered. However, within 1 week of wear, the patient returned and reported progressive clouding after several hours of use.
The Diagnostic Challenge
Cloudy vision with scleral lenses raises a wide differential diagnosis: midday fogging, tear reservoir debris, lens vault and clearance issues, corneal edema, or occult corneal pathology. With a complex post-RK cornea and limited prior success, narrowing the diagnosis efficiently was critical.
To that end, multimodal imaging with Anterion (Heidelberg Engineering) was employed. Two rapid scans—Cornea (see Figure 1) and Imaging Apps—provided remarkable clarity.
- Anterior Elevation (Best-Fit Sphere) Map: demonstrated central corneal flattening, consistent with classic post-RK biomechanics.
- Anterior Tangential Map: revealed the irregular astigmatism and asymmetric topography underlying her reduced eyeglasses and lens performance.
- Pachymetry Map: showed an unexpected finding—central corneal thickening juxtaposed with inferior-temporal thinning, a red flag for structural irregularity.
- Imaging App (High-resolution optical coherence tomography [OCT]; see Figure 2): identified thickening of Descemet’s membrane, visible as an irregular hyper-reflective posterior band, accompanied by mild central stromal haze.
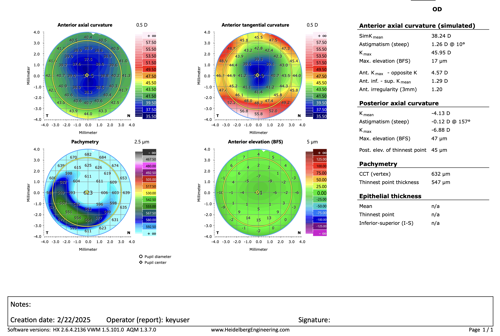
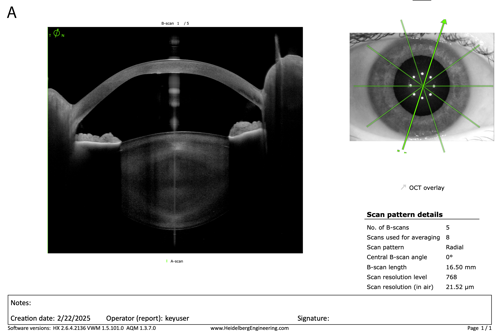
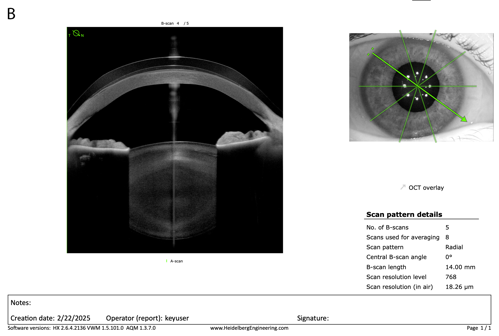
Together, these findings pointed toward 2 likely contributors to her visual decline: irregular astigmatism secondary to RK biomechanics and evolving endothelial disease with Descemet’s membrane changes.
Clinical Course and Outcome
Armed with this information, adjustments were made to her scleral lens design to optimize the material, the vault, and haptic alignment while addressing the contribution of corneal irregularity. A hypertonic saline solution was prescribed to use before and after contact lens wear. Treatment for ocular surface dryness was initiated concurrently.
With the modified scleral lens and new treatment plan, her best corrected visual acuity improved from 20/50 to 20/25 in the left eye with stable clarity throughout the wearing period. The patient, who had nearly resigned herself to a lifetime of frustration, left the office relieved and with renewed visual confidence.
Discussion
This case illustrates the enduring challenges of managing post-RK patients decades after surgery. The biomechanical instability of the cornea, coupled with progressive irregularity and endothelial changes, can make these eyes some of the most difficult to rehabilitate.
Traditional slit lamp examination and corneal topography often fall short in elucidating the full picture. Anterion’s multimodal capability—integrating topography, pachymetry, and high-resolution anterior segment OCT—proved invaluable in rapidly uncovering both surface and posterior corneal contributors to the patient’s complaints.
In a specialty contact lens practice, time is a scarce commodity. Unlike routine exams, visits often involve comprehensive medical evaluation and the iterative fitting process. Instruments that deliver fast, high-quality, multimodal data enable clinicians to move swiftly from uncertainty to action and improve patient outcomes while safeguarding practice efficiency.
Conclusion
For this patient, 2 decades of fluctuating post-RK vision, compounded by repeated fitting failures, culminated in a breakthrough enabled by advanced imaging. The ability of modern multimodal anterior segment systems to reveal pathology hidden in plain sight underscores their role as indispensable tools in specialty practices.
In our clinic, the Anterion has become a true workhorse—applied in nearly every anterior segment disease case—and has proven to be one of the single most impactful investments we have made in managing complex corneas.
This editorial content was supported via unrestricted sponsorship




