For those of us who manage many complex glaucoma patients, we often find conflicting data between the physical appearance of the optic nerve on clinical examination and the optical coherence tomography (OCT) and visual field findings. Sometimes these conflicts are easy to sort out. In other cases, however, it helps to know where to look.
Choose glaucoma software with a documented ability to evaluate several areas in the posterior pole related to structural changes associated with glaucoma. These areas include the Bruch’s membrane opening-minimum rim width (BMO-MRW) measurements, the macular region (including total retinal thickness as well as the ganglion cell layer [GCL] measurements), and the circumpapillary retinal nerve fiber layer (RNFL) measurements.
Patients can bring many different conditions with them when they present to the office, including a variety of posterior pole issues that can cloud the glaucoma evaluation. The ability to look at so many areas plays a role not only in the initial diagnostic phase of evaluating your glaucoma suspects but also in the long-term management of your glaucoma patients, particularly when ascertaining stability vs progression.
Figure 1 shows a multicolor image taken from the Spectralis ophthalmic imaging system (Heidelberg Engineering) of a patient with advanced glaucoma and a significant foveal-centered epiretinal membrane (ERM).

Just by looking at the image, we can see that evaluating this patient’s neurosensory retina in the macular region for indications of glaucomatous damage is going to be affected by the density of the ERM. Even the GCL, which typically is less affected than total retinal thickness, can show distortion, as seen in Figure 2. As plainly seen in this image, the temporal RNFL is also affected by the ERM, thereby making perioptic RNFL readings suspect at all diameters.

This rather dense ERM has eliminated any accurate information related to glaucomatous damage from 5 of the 6 regions able to be measured with the glaucoma software, with those being total retinal thickness, GCL thickness, and the 3 different diameter RNFL scans.
This leaves us just one remaining metric upon which to base clinical judgements for managing this patient’s glaucoma: the BMO-MRW readings, as shown in Figure 3.
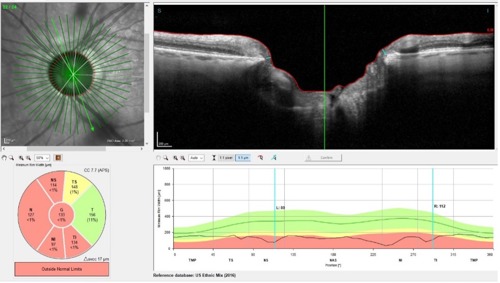
The BMO-MRW readings are taken as a series of radial scans from the center of the optic nerve outward, compensated for the foveal center, which usually sits slightly below horizontal. This scan area is completely unaffected by the ERM and therefore gives us reliable data with which to judge the stability of the glaucoma.
Clinical judgement is predicated upon knowing the facts of the case and, in particular, the data available to us to make educated clinical decisions as well as interpreting that data properly. This patient’s visual field test result may not help much in their glaucoma management given the ERM’s effect on fixation.
Offering outstanding clinical care is our goal, and knowing our options to deliver that care is our job.
This content is supported by Heidelberg




